Development, production and characterization of SARS-CoV-2 virus-like particles (Coronaviridae: Orthocoronavirinae: Betacoronavirus: Sarbecovirus)
- Authors: Latyshev O.E.1, Zaykova O.N.1, Eliseeva O.V.1, Savochkina T.E.1, Chernoryzh Y.Y.1, Syroeshkin A.V.2, Petrov G.V.2, Vorkunova G.K.1, Larichev V.F.1, Fediakina I.T.1, Cherepushkin S.A.1, Tsibezov V.V.1, Yuzhakova K.A.1, Kulikova N.Y.1, Lebedeva V.V.1, Yakunin D.Y.1, Kozlova A.A.1, Baranets M.S.1, Yurlov K.I.1, Lesnova E.I.1, Grebennikova T.V.1
-
Affiliations:
- National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
- Peoples’ Friendship University of Russia
- Issue: Vol 69, No 2 (2024)
- Pages: 175-186
- Section: ORIGINAL RESEARCHES
- URL: https://virusjour.crie.ru/jour/article/view/16637
- DOI: https://doi.org/10.36233/0507-4088-226
- EDN: https://elibrary.ru/gkxfed
- ID: 16637
Cite item
Abstract
Introduction. The COVID-19 pandemic caused by SARS-CoV-2 has created serious health problems worldwide. The most effective way to prevent the occurrence of new epidemic outbreaks is vaccination. One of the modern and effective approaches to vaccine development is the use of virus-like particles (VLPs).
The aim of the study is to develop a technology for production of VLP based on recombinant SARS-CoV-2 proteins (E, M, N and S) in insect cells.
Materials and methods. Synthetic genes encoding coronavirus proteins E, M, N and S were used. VLP with various surface proteins of strains similar to the Wuhan virus, Delta, Alpha and Omicron were developed and cloned into the pFastBac plasmid. The proteins were synthesized in the baculovirus expression system and assembled into VLP in the portable Trichoplusia ni cell. The presence of insertion in the baculovirus genome was determined by PCR. ELISA and immunoblotting were used to study the antigenic activity of VLP. VLP purification was performed by ultracentrifugation using 20% sucrose. Morphology was assessed using electron microscopy and dynamic light scattering.
Results. VLPs consisting of recombinant SARS-CoV-2 proteins (S, M, E and N) were obtained and characterized. The specific binding of antigenic determinants in synthesized VLPs with antibodies to SARS-CoV-2 proteins has been demonstrated. The immunogenic properties of VLPs have been studied.
Conclusion. The production and purification of recombinant VLPs consisting of full-length SARS-CoV-2 proteins with a universal set of surface antigens have been developed and optimized. Self-assembling particles that mimic the coronavirus virion induce a specific immune response against SARS-CoV-2.
Full Text
Introduction
According to WHO, as of November 8, 2023, there are more than 770 million confirmed cases of COVID-19 worldwide, including 6.9 million deaths. As of November 4, 2023, a total of 13,534,474,309 vaccine doses have been administered1. In Russia, there were 22,993 recovered, 5,042 hospitalized, and 63 deaths among the 34,191 identified COVID-19 cases in 44 weeks of 20232.
Vaccination is one of the most effective and affordable medical interventions that saves millions of lives every year [1]. Despite this, vaccine-preventable diseases reoccur and vaccine acceptability rates remain suboptimal for both routine vaccinations and those that are not included in the vaccination calendar [2]. Existing vaccines against SARS-CoV-2 are vector-based, mRNA-based, inactivated and virus-like particle (VLP) vaccines [3]. The efficacy of vaccines is affected by the continuous acquisition of viral mutations due to the inherent high error rate of viral RNA-dependent RNA polymerase and the existence of a highly variable receptor binding motif in the S protein [4].
A promising approach to creating effective vaccines is VLP-based vaccines, which are viral structural proteins capable of self-assembly, mimicking the virion but not carrying the viral genome. The VLP-based vaccines currently undergoing different phases of clinical trials are NVX-CoV2373 (Novavax) [5], Covifenz (Medicago) [6], ABNCoV2 (Radboud University) [7] and LYB001 (Yantai Patronus Biotech Co Ltd) [8]. However, only the S protein of SARS-CoV-2 is included in these vaccines. It seems more promising to develop vaccines based on the coronavirus 4 structural proteins to mimic the SARS-CoV-2 virion.
SARS-CoV-2 belongs to the β-Coronavirus genus of the Coronaviridae family of the Nidovirales order [9]. The SARS-CoV-2 genome is represented by RNA of a positive polarity of approximately 30,000 nucleotides in length and has approximately 82% sequence identity with SARS-CoV and MERS-CoV and > 90% sequence identity of key enzymes and structural proteins. The SARS-CoV-2 virion consists of four structural proteins, which include spike (S), envelope (E), membrane (M) and nucleocapsid (N) proteins [10, 11].
The N protein binds to the RNA of the virus to form a ribonucleocapsid inside the viral particle. Protein N is the most conserved protein of the coronavirus. Proteins E and M are relatively small proteins (75 and 222 amino acids in length respectively), that make up the viral envelope. Protein S makes up the spike on the surface of the virus. This protein plays a critical role in the pathogenesis of the virus. Receptor binding domain (RBD), a domain within this protein, is responsible for the binding of the viral particle to the cellular receptor. It is believed that antibodies which neutralize the virus are produced against this protein.
VLPs contain a large number of repetitive fragments of viral surface proteins, which are conformational viral epitopes that can induce T-cell and B-cell immune responses. During immunization, VLPs stimulate dendritic cells that capture the appropriate antigens for presentation to T- and B- lymphocytes [12].
The technology of VLP production allows to quickly change their composition, if necessary, according to the current epidemic situation. Since the gene encoding the coronavirus protein is initially located as DNA in the plasmid vector, its sequence can be modified by site-directed mutagenesis, and thus the antigenic composition of the vaccine can be adjusted, providing the formation of a wide range of antibodies against pandemic variants of SARS-CoV-2.
The aim of our study was to develop a technology for the production and purification of VLP based on recombinant E, M, N, and S SARS-CoV-2 proteins assembled in insect cells and to comprehensively characterize them.
Materials and methods
Molecular epidemiological studies
After comprehensive epidemiological studies to identify actual epidemically significant virus strains, virus gene sequences were selected and optimized for subsequent cloning into a donor plasmid and then into a bacmid [13].
Production of recombinant baculoviruses
The coding sequences were obtained synthetically, and the frequency of codon usage was optimized for expression in insect cell culture. The Bac-to-Bac expression system was used to create each genetic construct. The pFastBac transfer vector (donor plasmid) was used to produce a baculovirus expressing the M, E, N, and S proteins of topical coronavirus strains. This vector contains an expression cassette that contains flanking sequences of the Tn7 transposon in addition to the cloned genes. The recombinant transfer plasmid is used to transform DH10Bac Escherichia coli cells, which contain a modified baculovirus genome as a bacmid and a helper vector encoding the transposase enzyme. Recombinant DH10Bac clones were selected using the color test method. In selected white colonies, transfer of the expression cassette into the baculovirus genome was confirmed by PCR with primers, one specific to the cloned sequence and the other specific to the baculovirus genome.
Production and purification of VLP
Transfection of the transgenic Spodoptera frugiperda Sf-21 cell line was performed with purified bacmid DNA preparations containing codon-optimized coronavirus gene sequences using the cationic liposomal agent Cellfectin (Invitrogen, USA); two clones were used for each construct (seeding concentration of 5 × 105 cells/ml per 10 μl of bacmid). After transfection, two more passages were performed on Sf-9 cells.
VLPs were obtained by coinfection, i.e. simultaneous infection of a transviable insect cell line Trichoplusia ni (T.ni) with different combinations of recombinant baculoviruses. The transviable T.ni insect cell culture was cultured for 4 days after infection.
After culturing, the culture fluid (CF) was clarified by low-speed centrifugation to free cells and cellular debris at 1000 rpm for 5 min and 6000 rpm for 20 min, respectively (4 °C, Sorval SS34 rotor).
For isolation and purification of synthesized VLPs, clarified CF was layered in ultracentrifuge tubes on a layer of 6 ml of 20% sucrose solution (without mixing) prepared with TNS buffer (10 mM Tris-HCl, 140 mM NaCl, 10 mM CaCl2 pH 7.4). Centrifugation was performed for 2 hours at 28,000 rpm (Optima XE-100 centrifuge, SW 32Ti rotor, Beckman Coulter, +4 °C). The supernatant was removed, the precipitate was resuspended in TNC buffer and stored at 4 °C.
VLP properties
Electron microscopy. Purified VLPs in a volume of 3 μl were applied to a copper grid coated on a carbon substrate (Ted Pella, USA) and processed in a glow discharge atmosphere. They were incubated for 30 seconds at room temperature. Then a drop of 2% uranium acetate solution was applied and incubated for 30 seconds. The study was performed in a JEOL 2100 transmission electron microscope (JEOL, Japan) equipped with a lanthanum hexaborite cathode at an accelerating voltage of 200 kV. Images were acquired at ×25,000 magnification using a Gatan X100 CCD camera with a sensor size of 2000 × 2000 pixels (Gatan, USA).
VLP physical size. The physical size and distribution uniformity of VLPs in the purified suspension were determined by dynamic light scattering on a Malvern Zeta Sizer NANO instrument.
Protein concentration determination. The concentration of total protein in prepared purified VLP preparations was determined using a commercial BCA Protein Assay Kit (Thermo, USA).
Western blot. VLP structural proteins were analyzed by electrophoresis in 12% polyacrylamide gel with sodium dodecyl sulfate (PAAG-DSN) according to the method of Laemmli (1970) on a Mini-PROTEAN II device (Bio-Rad, USA) according to the manufacturer’s instructions. After electrophoresis, proteins were transferred to nitrocellulose membrane (0.45 μm, Schleicher & Schuell, Germany) in a Mini Trans-Blot cell (Bio-Rad, cat. no. 170-3930) according to the manufacturer’s method. Membranes were incubated with positive sera from COVID-19 reconvalescents and negative sera collected 20 years before the pandemic, at a dilution of 1 : 50. Antibodies that interacted with VLP proteins on the membrane were incubated with antibodies to human IgG conjugated with horseradish peroxidase (Sorbent, Russia) at a dilution of 1:200, and after incubation were detected using Super Signal West Femto Maximum (Thermo Scientific, USA) according to the manufacturer’s protocol. To detect the chemiluminescence signal, green-sensitive X-ray film (cat. No. 126041, Carestream, USA) was exposed on the membrane. The film was developed with the materials from VIPS-MED (Russia) according to the manufacturer’s method.
Neutralization reaction with sera from COVID-19 reconvalescents. Vero E6 cells were infected with SARS-CoV-2, and when cytopathic effect (CPE) was observed, the vial was frozen, thawed, CF was centrifuged at 3000 rpm, aliquoted, and frozen. Virus titer was determined by the finite dilution method, for which CF was added to a monolayer of Vero E6 cells at dilutions ranging from 10−1 to 10−8. The virus titer was considered to be the last dilution where CPE was detected. The 50% tissue cytopathic infectious dose (TCID50) was calculated according to the method of Reed and Mench. For the neutralization test (NT), a dilution of CF containing 100 TCID50 in 100 μl was used.
Blood sera from COVID-19 reconvalescents were prepared in dilutions from 1 : 10 to 1 : 1280 and added 100 µl each to the wells of a 96-well plate. 100 µl of virus-containing suspension was added to the serum dilutions and the mixture was incubated for one hour at 37 °C. The mixture was then transferred to a 96-well plate with a monolayer of Vero E6 cells. After 72 hours, the reaction was counted by viewing the wells of the plate in a microscope. If there are virus neutralizing antibodies in the serum, the virus will not induce cell CPE. The serum titer (last neutralizing dilution) was considered to be the dilution at which 100% cell protection (no CPE) was achieved.
Specific activity. The identity of antigens in the VLP to antigens in the SARS-CoV-2 viral particle was assessed by ELISA by interaction with antibodies to SARS-CoV-2 in the sera of COVID-19 reconvalescents previously characterized in NT. VLPs were sorbed into the wells of the plate for 18 hours at 4 °C. Then, sera from healthy individuals (negative control) and COVID-19 reconvalescentsat a dilution of 1 : 100 were added to the wells with sorbed VLPs and incubated for 1 hour at 37 °C. Then, antibodies to human IgG conjugated with horseradish peroxidase were added. (Sigma, USA). After incubation for 15 min (20–25 °C), the reaction was stopped with 1M H2SO4. The color intensity in the wells was determined on a spectrophotometer at a wavelength of 450 nm.
The level of VLP synthesis was assessed by quantification of S protein RBD by ELISA. Monoclonal antibodies (MCA) to RBD, obtained and characterized earlier in the laboratory, were used as capture and detection antibodies. The wells of immunoassay plates were sorbed with MCA at a concentration of 10 μg/mL for 18 hours at 4 °C. Then recombinant RBD was added at concentrations of 15.6; 31.25; 62.5; 125; 250; 500; 1000 ng/mL to construct a calibration curve and the tested VLP samples at dilution 1 : 200 to 1 : 400. After incubation for 1 hour at 37 °C, MCA peroxidase conjugate was added and incubated for 1 hour at 37 °C. Then a chromogen-substrate mixture with tetramethylbenzidine (Chema, Russia) was added. The reaction was incubated for 15 min (20–25 °C) and stopped with 1M H2SO4. The color intensity in the wells was determined on a spectrophotometer at a wavelength of 450 nm. The quantitative VLP content was expressed in RBD concentration, which was calculated from the optical density value using the calibration curve according to the following formula:
,
where: k – angle of the calibration curve;
n – dilution rate of the VLP sample.
VLP immunogenicity
To assess the immunogenicity of VLP, we studied the formation of humoral (NT and indirect ELISA as described above) and cellular immune response (lymphocyte blast-transformation test, LBTT) after triple immunization of golden hamsters (Mesocricetus auratus) by intramuscular injection of VLP in the concentration of 40 µg per animal.
Lymphocyte blast-transformation test
All manipulations were performed under sterile conditions. Spleens were extracted from hamsters and homogenized in 3 ml of pure RPMI-1640 medium in a sterile homogenizer. The cell suspension was centrifuged on a one-step ficoll-pak density gradient (HistoPaque-1077, Sigma, USA), the mononuclear cell fraction was isolated and washed twice in pure RPMI-1640 medium and placed in 96-well culture plates with a concentration of 105 cells in 100 μl per well. Stimulatory antigens were added 100 µl per well to cells to final concentrations. Splenocytes activated with Concanavalin A (ConA, 12.5 mg, PanEco, Russia) served as positive controls. Splenocytes from spleens of unimmunized hamsters; splenocytes without antigen stimulation, as well as splenocytes stimulated with nonspecific antigen (Crimean-Congo hemorrhagic fever virus) were used as negative controls. Cells were cultured in full-thickness RPMI-1640 medium, with 20% EFV, 2 mM glutamine, 4.5 g/L glucose, 50 μg/mL gentamicin, 0.2 units/mL insulin at 37 °C in an atmosphere of 5% CO2. Splenocyte proliferation was evaluated in the blast-transformation test after 4–5 days using an inverted microscope (×400 magnification). The results of LBTT were expressed as lymphocyte proliferation assay (LPA) – the ratio of the average number of blasts in the presence of stimulants to the average number of blasts in the absence of stimulants. The result was considered positive if the LPA exceeded 2.
The humoral immune response was assessed by indirect ELISA and NT methods with hamster sera after second and third immunizations. Cellular immunity (LBTT) was assessed after first and second immunizations.
Statistical processing of the results
Statistical processing of the results was performed using Prizm Graphpad 8.4.3 (Graph Pad Software, USA) and Statistica 12.6 (Stat Soft Inc., USA) programs. The results were considered statistically significant at p < 0.05.
Results
Molecular epidemiologic studies and production of recombinant baculoviruses
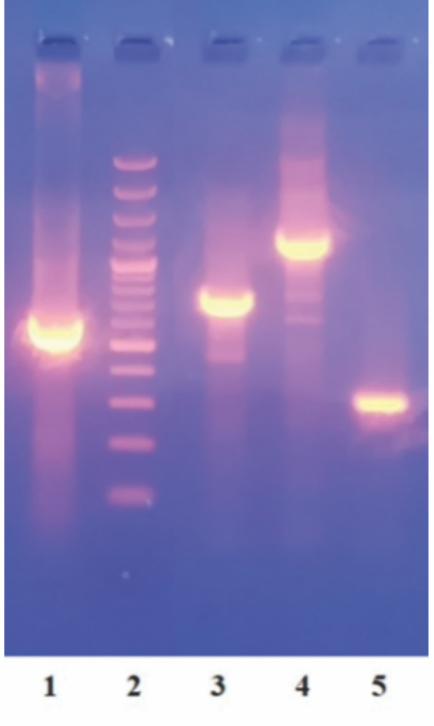
As a result of molecular epidemiologic studies [13], the S protein genes of 4 topical strains most prevalent in the Russian Federation and Europe – Wuhan-like, Delta, Alpha and Omicron and the E, M and N protein genes of SARS-CoV-2 were selected to produce recombinant proteins as vaccine antigens. The selected protein-coding sequences were optimized for expression in insect cells and cloned into the pFastBacDual transfer vector. Recombinant baculoviruses carrying the S protein genes of four different strains as well as the E, M, and N proteins of SARS-CoV-2 were obtained. The presence of gene insertions in recombinant baculoviruses was confirmed by PCR (Fig. 1).
Fig. 1. Gene inserts of the appropriate size in recombinant baculoviruses obtained as a result of PCR. 1 – diagnostic fragment of the S protein gene (597 bp); 2 – marker of molecular weights; 3 – insert containing the M protein gene (768 bp); 4 – insert containing the N protein gene (1359 bp); 5 – an insert containing the E protein gene (327 bp).
Рис. 1. Вставки генов соответствующего размера в рекомбинантных бакуловирусах, полученные в результате ПЦР. 1 – диагностический фрагмент гена белка S (597 п.н.); 2 – маркер молекулярных масс; 3 – вставка, содержащая ген белка M (768 п.н.); 4 – вставка, содержащая ген белка N (1359 п.н.); 5 – вставка, содержащая ген белка E (327 п.н.).
To optimize the conditions for the production of SARS-CoV-2 proteins, 3 passages of recombinant baculoviruses were used, which were infected with a transient culture of T.ni insect cells. The accumulation of target products was assessed by electrophoresis in polyacrylamide gel, as well as by enzyme immunoassay, in which the lysate of insect cells infected with recombinant baculoviruses at different doses was used as the material for the study, taking into account the duration of incubation (2‒5 days after infection of cells). Monoclonal antibodies to the RBD domain of the S-protein of SARS-CoV-2 were used as detection antibodies. As a result of this work, the optimal clones for each construct were determined, as well as the duration of incubation of insect cell culture infected with different recombinant baculoviruses. The obtained data were used in experiments aimed at optimizing the parameters of coinfection-simultaneous infection of a transviable insect cell line T.ni with different combinations of recombinant baculoviruses. In the first step, recombinant baculoviruses were used at the same infection dose (0.02 TCD50). As a result, 4 different VLPs containing different S proteins of SARS-CoV-2 were constructed: each particle had one of the 4 S proteins of the actual strains, as well as E, M and N proteins on its surface, as confirmed by immunoblotting (Fig. 2).
Fig. 2. Western blot of recombinant VLP proteins after treatment with positive (a) and negative serum (b). Tracks: 1 – negative control (cells T.ni); 2 – N; 3 – M; 4 – E; 5 – S (Wuhan-like virus); 6 – S (Omicron); 7 – S (Delta); 8 – S (Alpha); 9 – positive control (SARS-CoV-2).
Рис. 2. Вестерн-блот рекомбинантных белков VLP после обработки положительной (а) и отрицательной сывороткой (б). Дорожки: 1 – отрицательный контроль (клетки T.ni); 2 – N; 3 – M; 4 – E; 5 – S (подобный вирусу Ухань), 6 – S (Omicron); 7 – S (Delta); 8 – S (Alpha); 9 – положительный контроль (SARS-CoV-2).
Thus, using western blot, it was proved that the protein bands accounted for in the samples of recombinant VLP proteins are specific and correspond to spike (S) glycoprotein, small envelope (E) glycoprotein, membrane (M) glycoprotein and nucleocapsid (N) protein.
Characterization of purified VLP preparations
The morphology, physical size and distribution uniformity of purified VLPs were determined by electron microscopy and by dynamic light scattering on a Malvern Zeta Sizer NANO instrument (Fig. 3).
Fig. 3. Morphology and physical dimensions of purified VLPs. a – electron microscopy of VLP; b – histogram of VLP size distribution.
Рис. 3. Морфология и физические размеры очищенных VLP. а – электронная микроскопия VLP; б – гистограмма распределения VLP по размеру.
The specificity and synthesis level of purified VLPs were evaluated by the concentration of total protein and the concentration of receptor-binding RBD domain of S protein. The obtained VLPs were considered to be specifically active if the RBD content was greater than 5 μg/mL. Based on electron microscopy data, if more than 90% of the obtained VLPs were collected correctly and not degraded, the concentration of total protein in the purified VLP preparations could be taken as the VLP concentration. Table 1 shows the average values of VLP content obtained from 1 L of culture fluid.
Table 1. Efficiency of VLP synthesis of 4 coronavirus strains containing S protein: similar to the Wuhan-like virus, Delta, Alpha and Omicron
Таблица 1. Эффективность синтеза VLP, содержащих S-белок 4 штаммов коронавируса: подобный вирусу Ухань, Delta, Alpha и Omicron
VLP SARS-CoV-2 | Total protein content in purified VLPs obtained from 1 liter of culture fluid, mg (n = 10) Содержание общего белка в очищенных VLP, полученных из 1 л КЖ, мг (n = 10) |
Wuhan-like virus/ Подобный вирусу Ухань (n = 8) | 5,6 ± 1,9 |
Delta (n = 11) | 5,9 ± 1,7 |
Alpha (n = 11) | 6,2 ± 1,2 |
Omicron (n = 8) | 5,5 ± 1,9 |
Assessment of VLP immune specificity using sera from healthy individuals and COVID-19 reconvalescents
The synthesized and purified VLPs mimic the structure of the SARS-CoV-2 virion, with antigenic determinants similar to those of SARS-CoV-2. The results of the immune specificity study (Fig. 4) with sera of COVID-19 reconvalescents indicate the specificity of the obtained VLPs.
Fig. 4. Results of a study of the immune specificity of VLP in ELISA with human sera characterized by NT. The X-axis shows human sera characterized in NT; the Y-axis shows optical density at a wavelength of 450 nm, legend – VLP at concentrations of 8, 2, 0.5 and 0.125 micrograms/well: otp 1 – serum negative in NT; otp 2 – serum negative in NT collected more than 20 years ago; 1 : 320 – serum positive in NT, titer 1 : 320; 1 : 160 –serum positive in NT, titer 1 : 160; 1 : 80 – serum positive in NT, titer 1 : 80.
Рис. 4. Результаты исследования иммуноспецифичности VLP в ИФА с сыворотками крови лиц, охарактеризованных в РН. По оси абсцисс представлены сыворотки крови, охарактеризованные в РН; по оси ординат – оптическая плотность при длине волны 450 нм, легенда – VLP в концентрациях 8, 2, 0,5 и 0,125 мкг/лунку: отр 1 – сыворотка, отрицательная в РН; отр 2 – сыворотка, отрицательная в РН, взятая более 20 лет назад; 1 : 320 – сыворотка, положительная в РН, титр 1 : 320; 1 : 160 – сыворотка, положительная в РН, титр 1 : 160; 1 : 80 – сыворотка, положительная в РН, титр 1 : 80.
Thus, the obtained VLPs are effectively recognized by specific antibodies from the sera of COVID-19 reconvalescents. There was a correlation between the titer in the neutralization reaction and the optical density in the enzyme immunoassay, which proves the presence of specific interacting antibodies with VLPs.
Immunogenicity of VLP
To evaluate the immunogenicity of VLP, we studied the formation of humoral (NT and ELISA) after 2 and 3 immunizations and cellular immunity (LBTT) after 1 and 2 immunizations of golden hamsters (Mesocricetus auratus) by intramuscular administration of VLP preparation at a concentration of 40 μg /dose. Using a set of methods, the results were obtained and presented as mean ± standard deviation (M ± SEM) in Table 2.
Table 2. Results of the presence of specific IgG, neutralizing antibodies and LPAs in the serum and blood of golden hamsters immunized intramuscularly with VLP at a concentration of 40 μg /dose, M ± SEM
Таблица 2. Результаты наличия специфических IgG, нейтрализующих антител и ИСП в сыворотке крови и крови золотистых хомячков, иммунизированных внутримышечно VLP в концентрации 40 мкг/доза, M ± SEM
Immunization Иммунизация | LPA ИСП | Immunization Иммунизация | NT, val. РН, обр.зн. | ELISA, opt.dens. ИФА, опт.пл. | Reciprocal titer value ИФА, обр.зн. титра ELISA |
1 | 0,4 ± 0,01 | 2 | 340 ± 173 | 1,094 ± 0,26 | 12,800 |
2 | 8,9 ± 0,91* | 3 | 1280 ± 0* | 1,613 ± 0,01 | 12,800 |
Note. * – values significantly different from the value of the previous immunization (p < 0.05).
Примечание. * – значения, достоверно отличающиеся от значения предыдущей вакцинации (р < 0,05).
It is shown that twofold immunization is sufficient for the formation of cellular immunity. After the second immunization there is a statistically significant, almost twenty-fold increase in LPA (8.9 ± 0.91) compared to the first immunization (0.4 ± 0.01) (p < 0.05). The study of humoral immunity showed that specific viral neutralizing IgG antibodies are detected after the second and third immunization of hamsters. IgG level does not change depending on the number of immunizations (OD: 1.094 ± 0.26 and 1.613 ± 0.01 after second and third immunizations, respectively) (p > 0.05). At the same time, there was a significant increase in viral neutralizing antibodies after the third immunization almost 4 times compared to the second immunization (OD: 1280±0 and 340±173 after second and third immunizations, respectively) (p < 0.05). Thus, the obtained results indicate the formation of specific humoral and cellular response in all immunized hamsters studied in response to intramuscular injection of VLP at a concentration of 40 μg /dose.
Discussion
The COVID-19 pandemic has had a serious impact on the world from both a social and economic standpoint. From the beginning, SARS-CoV-2, the COVID-19 pathogen, has been constantly changing and continues to evolve to this day. To date, many SARS-CoV-2 genetic variants have been reported in different regions of the world. There are serious concerns about the efficacy of existing vaccines against new variants of the virus. Taking this into account, the problem of developing new vaccine preparations that not only induce an effective immune response but also induce cross-reactive immunity, providing protection against new SARS-CoV-2 variants, remains extremely urgent [14]. The studies of unique SARS-CoV-2 genetic variants circulating in Europe and in the Russian Federation have shown which antigenic determinants should be taken into account when developing a vaccine preparation. The variability of the SARS-CoV-2 genome during the spread of COVID-19 was analyzed.
In the present study, VLPs mimicking SARS-CoV-2 virion containing 4 structural proteins – E, M, N and S of SARS-CoV-2 were obtained. At the same time, surface determinants are represented by S proteins of actual clades – Wuhan-like strain (19A), Indian (Delta), British (Alpha) and Omicron. Therefore, a vaccine based on the derived VLPs provides broad-spectrum antibody formation and will help prevent infection caused by different strains of SARS-CoV-2, as well as generate an immune response similar to that induced during natural infection [15]. A significant advantage of VLP-based vaccines is the absence of genetic material, which eliminates the possibility of viral genome replication. Furthermore, antigens presented on the surface of VLPs in their native conformation are more stable than in the form of subunits, which leads to the use of smaller doses of antigen required to trigger a protective immune response.
Between the Wuhan and Omicron strains, T cell epitopes are highly conserved, while many neutralizing antibody epitopes are located in the spike-trimer variable regions, and Omicron BA-1 to BA.5 subvariants, have mutations in the RBD, which reduces the neutralizing ability of antibodies generated by current vaccines [15, 16]. This emphasizes the need for new approaches in vaccine development and the addition of other antigens such as E, M, N proteins that are less mutated than S in the COVID-19 vaccine formulation. Because antibody response is less effective against novel virus variants than T cell response, a vaccine that induces both cellular and humoral immunity may have a significant advantage.
Therefore, synthesized VLPs that mimic the SARS-CoV-2 virion, contain 4 structural proteins, E, M, N, and S of SARS-CoV-2 topical clades, and stimulate the formation of humoral and cellular immunity are promising antigens for further development of a VLP-based vaccine that will provide effective protection against SARS-CoV-2 [15, 16].
The baculovirus expression system used in this work in insect cells to create VLPs has several advantages: baculoviruses do not infect humans, making the work safe; insect cells grow in serum-free medium that is free of animal products, retroviruses and is not oncogenic; and VLP synthesis in a baculovirus expression system can be scaled and optimized for commercial production of immunobiological drugs.
Nowadays, approved and commercially available VLP-based vaccines include vaccines against human papillomavirus (Cervarix Gardasil, Gardasil 9), against hepatitis B virus (Engerix Glaxo Smith Kline, Recombivax) [17]. Against COVID-19 infection, the VLP vaccine 6p-VLP-58-1023-Al-K3 with CpG ODN/alum adjuvant expressing all four structural protein antigens of SARS-CoV-2 has shown immunogenic and protective properties in mice, rats and ferrets [18]. This vaccine has undergone phase 1 clinical trials in humans [19].
Conclusion
The system of synthesis and purification of virus-like particles from recombinant proteins synthesized in baculovirus expression system was optimized. As a result, stable virus-like particles consisting of four recombinant SARS-CoV-2 proteins, E, M, N and S, mimicking the SARS-CoV-2 virion, capable of inducing a specific immune response against SARS-CoV-2 were obtained. The specificity of the obtained VLPs was proved. The developed VLPs can be used as an antigen in an immunobiologic drug product for COVID-19 prophylaxis.
1 World Health Organization. COVID-19. Available at: https://covid19.who.int/
2 In Russia, 22,993 people recovered in a week. Working hours: https://объясняем .Russian Federation/stopkoronavirus/v-rossii-za-nedelyu-vyzdorovelo-22-993-cheloveka/
About the authors
Oleg E. Latyshev
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: oleglat80@mail.ru
ORCID iD: 0000-0002-5757-3809
PhD, Senior Scientist, Laboratory of molecular diagnostics
Russian Federation, 123098, MoscowOlga N. Zaykova
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: zaykova_o_n@mail.ru
ORCID iD: 0000-0003-4708-2069
Researcher at the Laboratory of Molecular Diagnostics
Russian Federation, 123098, MoscowOlesya V. Eliseeva
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: olesenka80@mail.ru
ORCID iD: 0000-0002-0723-9749
PhD, Senior Scientist, Laboratory of molecular diagnostics
Russian Federation, 123098, MoscowTatyana E. Savochkina
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: tasavochkina@yandex.ru
ORCID iD: 0000-0003-4366-8476
Researcher, Laboratory of Molecular Diagnostics
Russian Federation, 123098, MoscowYana Yu. Chernoryzh
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: revengeful_w@mail.ru
ORCID iD: 0000-0001-9848-8515
Candidate of Medical Sciences, Researcher, laboratory of molecular diagnostics
Russian Federation, 123098, MoscowAnton V. Syroeshkin
Peoples’ Friendship University of Russia
Email: syroeshkin-av@rudn.ru
ORCID iD: 0000-0003-3279-7520
Doctor of Biological Sciences, Professor, Head of the Department of Pharmaceutical and Toxicological chemistry
Russian Federation, 117198, MoscowGleb V. Petrov
Peoples’ Friendship University of Russia
Email: petrov-gv@rudn.ru
ORCID iD: 0009-0004-1123-7393
3rd year PhD Student, Assistant at the Department of Pharmaceutical and Toxicological chemistry
Russian Federation, 117198, MoscowGalina K. Vorkunova
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: g.k.vorkunova@gmail.com
ORCID iD: 0000-0003-1346-3744
Doctor of Biological Sciences, Leading Researcher, Laboratory of Molecular Diagnostics National Research Center
Russian Federation, 123098, MoscowVictor F. Larichev
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: vlaritchev@mail.ru
ORCID iD: 0000-0001-8262-5650
Doctor of Med. Sci, Leading Researcher, laboratory of biology and indication of arbovirus infections
Russian Federation, 123098, MoscowIrina T. Fediakina
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: irfed2@mail.ru
ORCID iD: 0000-0001-6421-9632
PhD, Lead Researcher of laboratory of viral ecology
Russian Federation, 123098, MoscowStanislav A. Cherepushkin
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: cherepushkin1@gmail.com
ORCID iD: 0000-0002-1734-5369
Researcher of laboratory of molecular diagnostics
Russian Federation, 123098, MoscowValeriy V. Tsibezov
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: tsibezov@yandex.ru
ORCID iD: 0000-0003-2150-5764
PhD, Leading Researcher of laboratory of specific virus prevention products
Russian Federation, 123098, MoscowKsenia A. Yuzhakova
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: chekh-ks@mail.ru
ORCID iD: 0000-0003-3130-5029
Researcher of laboratory of molecular diagnostics
Russian Federation, 123098, MoscowNadezhda Yu. Kulikova
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: nad007@rambler.ru
ORCID iD: 0000-0002-3008-3383
Researcher of laboratory of molecular diagnostics
Russian Federation, 123098, MoscowVarvara V. Lebedeva
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: lebedevavv@yandex.ru
ORCID iD: 0000-0002-3088-0403
Researcher of laboratory of molecular diagnostics
Russian Federation, 123098, MoscowDmitriy Yu. Yakunin
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: yd364@mail.ru
ORCID iD: 0009-0009-4531-5739
Graduate student of laboratory of molecular diagnostics
Russian Federation, 123098, MoscowAlina A. Kozlova
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: malinkakozlova88@gmail.com
ORCID iD: 0000-0003-2749-3258
PhD, researcher, laboratory of biology and indication of arbovirus infections
Russian Federation, 123098, MoscowMarina S. Baranets
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: shizotorex@mai.ru
ORCID iD: 0000-0002-3466-3588
PhD, researcher, laboratory of biology and indication of arbovirus infections
Russian Federation, 123098, MoscowKirill I. Yurlov
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: kir34292@yandex.ru
ORCID iD: 0000-0002-4694-2445
Researcher, laboratory of cellular engineering
Russian Federation, 123098, MoscowEkaterina I. Lesnova
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Email: wolf252006@yandex.ru
ORCID iD: 0000-0002-2801-6843
Researcher, laboratory of Molecular Diagnostics
Russian Federation, 123098, MoscowTatyana V. Grebennikova
National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya of the Ministry of Health of the Russian Federation
Author for correspondence.
Email: t_grebennikova@mail.ru
ORCID iD: 0000-0002-6141-9361
Doctor of Biological Sciences, Professor, Corresponding Member RAS, deputy Director for Science of the Division of the Ivanovsky Virology Institute Head of the Control Center of National Research Center for Epidemiology and Microbiology named after Honorary Academician N.F. Gamaleya
Russian Federation, 123098, MoscowReferences
- Rappuoli R., Pizza M., Del Giudice G., De Gregorio E. Vaccines, new opportunities for a new society. Proc. Natl Acad. Sci. USA. 2014; 111(34): 12288–93. https://doi.org/10.1073/pnas.1402981111
- Omer S.B., Salmon D.A., Orenstein W.A., deHart M.P., Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N. Engl. J. Med. 2009; 360(19): 1981–8. https://doi.org/10.1056/NEJMsa0806477
- Li M., Wang H., Tian L., Pang Z., Yang Q., Huang T., et al. COVID-19 vaccine development: milestones, lessons and prospects. Signal Transduct. Target Ther. 2022; 7(1): 146. https://doi.org/10.1038/s41392-022-00996-y
- Lou F., Li M., Pang Z., Jiang L., Guan L., Tian L., et al. Understanding the secret of SARS-CoV-2 variants of concern/interest and immune escape. Front. Immunol. 2021; 12: 744242. https://doi.org/10.3389/fimmu.2021.744242
- Heath P.T., Galiza E.P., Baxter D.N., Boffito M., Browne D., Burns F., et al. Safety and efficacy of NVX-CoV2373 COVID-19 vaccine. N. Engl. J. Med. 2021; 385(13): 1172–83. https://doi.org/10.1056/NEJMoa2107659
- Chhibber S., Jain D. Plant-based vaccines to combat COVID-19: strategies, status and prospects. Purva Mimaansa. 2022; 13: 25–30.
- Smit M.J., Sander A.F., Ariaans M.B.P.A., Fougeroux C., Heinzel C., Fendel R., et al. First-in-human use of a modular capsid virus-like vaccine platform: an open-label, non-randomised, phase 1 clinical trial of the SARS-CoV-2 vaccine ABNCoV2. Lancet Microbe. 2023; 4(3): e140–8. https://doi.org/10.1016/S2666-5247(22)00337-8
- Li Y., Zhang Y., Zhou Y., Li Y., Xu J., Ai Y., et al. An RBD virus-like particle vaccine for SARS-CoV-2 induces cross-variant antibody responses in mice and macaques. Signal Transduct. Target. Ther. 2023; 8(1): 173. https://doi.org/10.1038/s41392-023-01425-4
- V’kovski P., Kratzel A., Steiner S., Stalder H., Thiel V. Coronavirus biology and replication: implications for SARS-CoV-2. Nat. Rev. Microbiol. 2021; 19(3): 155–70. https://doi.org/10.1038/s41579-020-00468-6
- Jackson C.B., Farzan M., Chen B., Choe H. Mechanisms of SARS-CoV-2 entry into cells. Nat. Rev. Mol. Cell Biol. 2022; 23(1): 3–20. https://doi.org/10.1038/s41580-021-00418-x
- Hu B., Guo H., Zhou P., Shi Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021; 19(3): 141–54. https://doi.org/10.1038/s41579-020-00459-7
- Eggenhuizen P.J., Ng B.H., Chang J., Fell A.L., Cheong R.M.Y., Wong W.Y., et al. BCG vaccine derived peptides induce SARS-CoV-2 T cell cross-reactivity. Front. Immunol. 2021; 12: 692729. https://doi.org/10.3389/fimmu.2021.692729
- Ozhmegova E., Savochkina T.E., Prilipov A.G., Tikhomirov E.E., Larichev V.F., Sayfullin M.A., et al. Molecular epidemiological analysis of SARS-CoV-2 genovariants in Moscow and Moscow region. Voprosy virusologii. 2022; 67(6): 496–505. https://doi.org/10.36233/0507-4088-146 https://elibrary.ru/crgiwk (in Russian)
- Rambaut A., Holmes E.C., O’Toole Á., Hill V., McCrone J.T., Ruis C., et al. A dynamic nomenclature proposal for SARS-CoV-2 to assist genomic epidemiology. Nat. Microbiol. 2020; 5(11): 1403–7. https://doi.org/10.1038/s41564-020-0770-5
- Choi S.J., Kim D.U., Noh J.Y., Kim S., Park S.H., Jeong H.W., et al. T cell epitopes in SARS-CoV-2 proteins are substantially conserved in the Omicron variant. Cell. Mol. Immunol. 2022; 19(3): 447–8. https://doi.org/10.1038/s41423-022-00838-5
- Syed A.M., Ciling A., Taha T.Y., Chen I.P., Khalid M.M., Sreekumar B., et al. Omicron mutations enhance infectivity and reduce antibody neutralization of SARS-CoV-2 virus-like particles. Proc. Natl Acad. Sci. USA. 2022; 119(31): e2200592119. https://doi.org/10.1073/pnas.2200592119
- Hemmati F., Hemmati-Dinarvand M., Karimzade M., Rutkowska D., Eskandari M.H., Khanizadeh S., et al. Plant-derived VLP: a worthy platform to produce vaccine against SARS-CoV-2. Biotechnol. Lett. 2022; 44(1): 45–57. https://doi.org/10.1007/s10529-021-03211-0
- Yilmaz I.C., Ipekoglu E.M., Bulbul A., Turay N., Yildirim M., Evcili I., et al. Development and preclinical evaluation of virus-like particle vaccine against COVID-19 infection. Allergy. 2022; 77(1): 258–70. https://doi.org/10.1111/all.15091
- National Library of Medicine. Study of a severe acute respiratory syndrome CoV-2 (SARS-CoV-2) virus-like particle (VLP) vaccine in healthy adults (COVID-19); 2022. Available at: https://clinicaltrials.gov/study/NCT04818281
Supplementary files