Characteristics of the epidemic process of measles, rubella and mumps in Moscow and assessment of their seroprevalence at the present stage
- Authors: Simakova Y.V.1, Gushchin V.A.1,2,3, Semenenko T.A.1,2, Ogarkova D.A.1, Kleymenov D.A.1, Nozdracheva A.V.1, Manuylov V.A.1,4, Tkachuk A.P.5, Gintsburg A.L.1,2
-
Affiliations:
- National Research Centre for Epidemiology and Microbiology Named After Honorary Academician N. F. Gamaleya of the Ministry of Health of the Russian Federation
- I.M. Sechenov First Moscow State Medical University of the Ministry of Health of the Russian Federation (Sechenov University)
- Lomonosov Moscow State University
- Novosibirsk State University
- National Medical Research Center for Phthisiopulmonology and Infectious Diseases of the Ministry of Health of the Russian Federation
- Issue: Vol 70, No 2 (2025)
- Pages: 133-146
- Section: ORIGINAL RESEARCHES
- URL: https://virusjour.crie.ru/jour/article/view/16700
- DOI: https://doi.org/10.36233/0507-4088-282
- EDN: https://elibrary.ru/vhxaqq
- ID: 16700
Cite item
Abstract
Introduction. The problem of vaccine-preventable infections requires assessing the state of herd immunity through serological monitoring.
The aim. To study the epidemiological features of measles, rubella and mumps and to estimate their seroprevalence in the last decade in Moscow.
Materials and methods. Forms of federal statistical observation; State reports «On the state of sanitary and epidemiological well-being of the Moscow population»; official EMISS data for 2012–2023 were used to conduct a retrospective analysis of incidence. Blood serum samples (n = 7458) from healthy individuals stratified by age were tested for the presence of IgG antobodies to measles, rubella and mumps using the ELISA. Statistical data processing was performed using Microsoft Excel and SPSS Statistics v.27 (IBM).
Results. The analysis of epidemiological situation in Moscow in 2012–2023 revealed the presence of multidirectional trends: wave-like increase in the incidence of measles, stabilization of rubella cases registration and unstable incidence of mumps with an upward trend. A high prevalence of IgG antibodies to rubella virus was determined, preventing the spread of infection among the population. The formed level of herd immunity to mumps does not allow reducing the incidence to sporadic cases. The observed trend of increasing measles incidence can be explained by the accumulation of non-immune individuals among the population.
Conclusion. The significant proportion of seronegative individuals indicate the necessity to adjust vaccination prevention tactics and implement measures for mopping-up and catch-up immunization of the population against measles and mumps, especially in risk age groups.
Keywords
Full Text
Introduction
Global experience in the control of infectious diseases has shown that immunization of the population is one of the main means of controlling the epidemic process of many infections. In particular, currently controllable infections include measles, rubella and mumps, each of which in the pre-vaccination period caused significant economic damage and was characterized by high mortality. Established by the World Health Organization (WHO) in 1974, the Expanded Program on Immunization (EPI) aimed to achieve high preventive vaccination coverage and to implement a system of effective epidemiological surveillance in participating countries, regardless of their geographic location or socioeconomic status1. Over the past 50 years, efforts to implement the EPI have saved more than 154 million lives worldwide and contributed to changing the global health landscape2.
After the introduction of vaccination against measles (1967), mumps (1981) and rubella (1997) into Russia’s National Immunization Schedule, the incidence of these infections, as well as mortality from them, began to decline systematically. These diseases are traditionally considered as viral infections with a very similar epidemic process and have a number of common characteristics: airborne transmission mechanism; low resistance of the pathogen in the environment; protective post-infection immunity; similar prophylaxis tactics with attenuated vaccines, etc. [1]. The WHO Regional Office for Europe developed and implemented a strategic program to eliminate measles and rubella by 2010, which consisted in interrupting the local spread of infection due to a high level of herd immunity, while imported cases and limited outbreaks may be registered. Achieving and sustaining high vaccination coverage with two doses of measles vaccine (> 95%) and at least one dose of rubella vaccine was essential for the program’s implementation3.
However, as the number of rubella cases decreased to a single case, since 2011, measles incidence has been rising in many countries of the world, including the Russian Federation. The extension of the WHO Measles and Rubella Elimination Program to 20204, and then to 20305 has not made significant changes, and the medical and social significance of these infections, especially measles, remains at a high level [2–4]. In 2023, another cyclical rise in measles incidence was observed in the Russian Federation. There were 13,083 cases of measles, the incidence rate was 8.92 cases per 100,000 population, which is 7 times higher than the average annual rate (AAR) (AAR – 1.28 per 100,000 population)6. According to WHO information, Russia ranked 3rd in the European Region in the number of detected measles cases from July 2023 to June 20247.
Most of the works devoted to the problem of morbidity of vaccine-preventable infections at the stage of their elimination are focused on the issues related to the study of regularities of the epidemic process development, as well as the analysis of the population coverage by preventive vaccinations according to statistical reporting data. Insufficient objectivity in assessing the quality of immunoprophylaxis based on documentation alone can be associated with a lack of cold chain compliance during drug transportation, low effectiveness of vaccines, violation of immunization schemes, increase in the number of vaccination refusals, etc. [5, 6]. In this regard, tracking the state of herd and individual specific immunity through serologic monitoring, which is a component of the information support subsystem of the epidemiologic surveillance system of vaccine prophylaxis, becomes especially important in the context of heterogeneity of the vaccinated population [7, 8].
The methodological guidelines for the organization and conduct of serological monitoring for the state of herd immunity to infections controlled by means of specific prophylaxis consider indicator groups of the population8 to assess the effectiveness of vaccination measures, but at the present stage there is a need to examine a wider population, in some cases without information on vaccination history, because not all (especially adults) have vaccination passports, where these data are reliably reflected.
The aim of the study was to investigate the epidemiological features of measles, rubella and mumps and to assess the level of their seroprevalence in the last decade, using the example of a large metropolitan area – the city of Moscow.
Materials and methods
The material for the retrospective analysis of incidence were the federal state statistical observation forms No. 2 “Information on Infectious and Parasitic Diseases”, No. 5 “Information on Preventive Vaccinations”, No. 6 “Information on Contingents of Children and Adults Vaccinated Against Infectious Diseases”, data from the state reports “On the State of Sanitary and Epidemiologic Welfare of the Population in the Russian Federation” and “On the State of Sanitary and Epidemiologic Welfare of the Population in the City of Moscow”, as well as from the official reports “On the State of Sanitary and Epidemiologic Welfare of the Population in the City of Moscow”.
In order to assess herd immunity to various infections in Russia, studies were organized with the formation of a bank containing 28,395 blood serum samples collected from the conditionally healthy population without age restriction in the period from 2018 to the beginning of 2020. The study was conducted in accordance with the principles of the Declaration of Helsinki. All participants (donors of blood serum samples) gave voluntary informed consent to participate in the study. The study was approved by the Independent Interdisciplinary Committee for Ethical Review of Clinical Trials (Moscow, Russia) (permission No. 17 of 16.11.2018). The present study describes only the data obtained during the study of 7458 blood serum samples obtained in 2019 from conditionally healthy donors living in the territory of Moscow and the Moscow region for the presence of specific antibodies of class G (IgG) to measles, rubella and mumps viruses. When assessing the level of herd immunity, the subjects were stratified into age groups: 0–1 years, 2–5 years, 6–10 years and further with a step of 5 years up to 60 years, 60–70 years and over 71 years of age. The study was organized and conducted in accordance with the methodological guidelines for organizing and conducting serological monitoring for the state of collective immunity to infections controlled by means of specific prophylaxis8. Information on vaccination status and history of the studied infections was obtained by questioning volunteers. Blood serum samples were analyzed by enzyme-linked immunosorbent assay (ELISA) using domestic test systems VectoCory-IgG, VectoRubella-IgG and VectoParotitis-IgG (Vector-Best, Russia), following the manufacturer’s instructions. According to the instructions for use of the test systems, the following serum IgG antibody levels were considered as positive results: ≥ 0.18 IU/mL for measles, ≥ 10 IU/mL for rubella, ≥ 29.27 CU/mL for mumps.
Statistical processing of data was performed using Microsoft Excel and SPSS Statistics ver. 27 (IBM, USA). For epidemiologic analysis, absolute and relative incidence indices were used with the construction of confidence intervals using the Wilson method. To test the significance of differences in results between groups of examined individuals, the χ2 criterion with Yates correction was used when appropriate criteria were available. The association coefficient (Ka) was used to analyze the interaction between binary parameters. Logistic regression models were constructed to analyze the interaction of more than two parameters with each other. Nagelkerke’s coefficient of determination R2 was used to analyze the quality of the model.
Results
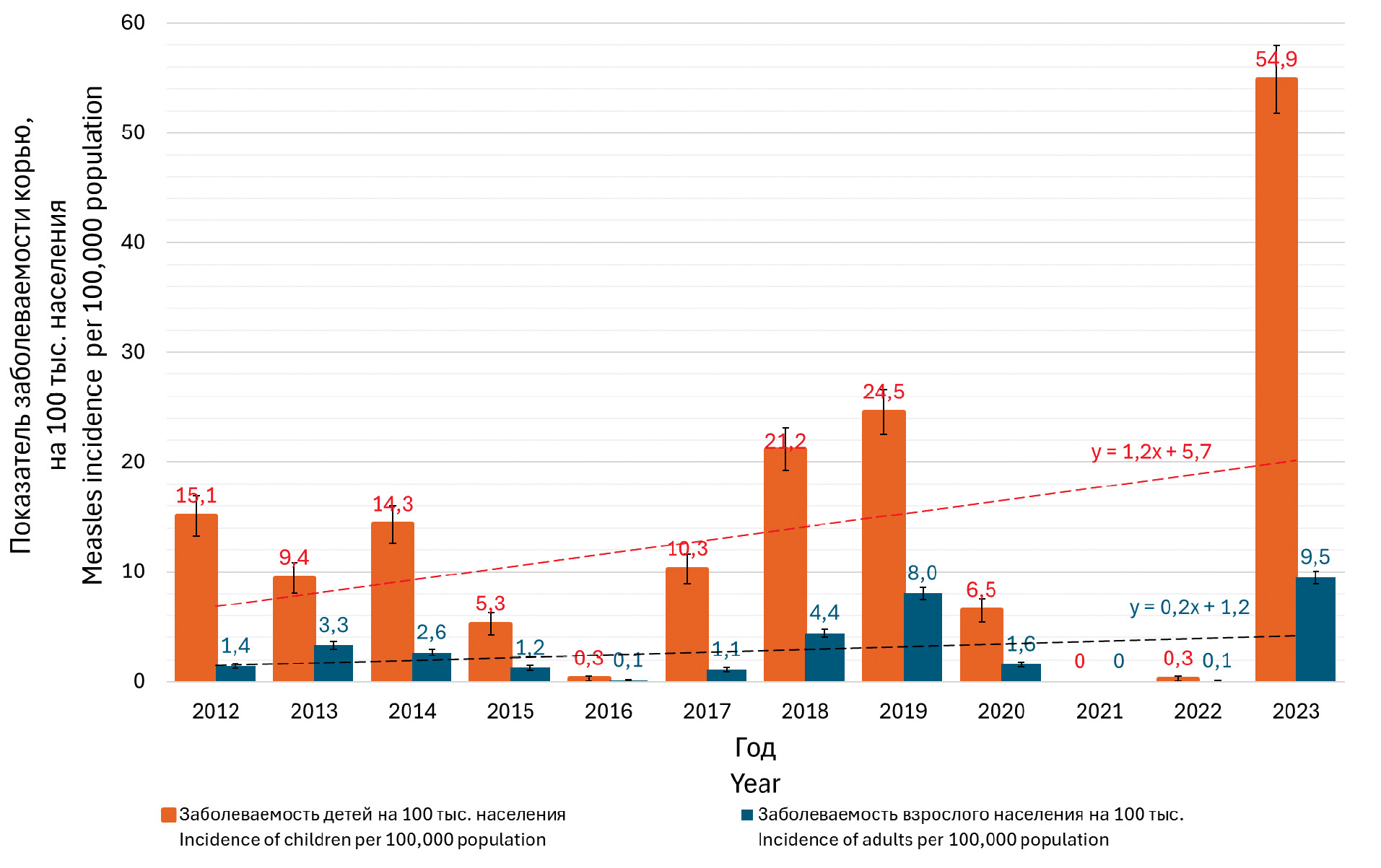
Retrospective epidemiological analysis of measles incidence in Moscow against the background of high vaccination coverage indicates different intensity of the epidemic process, which was characterized by periodic rises and declines: In the years of rise (2018, 2019 and 2023), the adult measles incidence rate reached 4.4 and 8.0 and 9.5 per 100,000 population, respectively; in the decline years (2016, 2021 and 2022), the rate decreased to 0.1, 0 and 0.1 per 100,000 population (Fig. 1). In the pediatric population, the variation in rates was even greater: 21.2, 24.5 and 54.9 per 100,000 population in the up years and 0.3, 0 and 0.3 per 100,000 population in the down years, respectively (Fig. 1). Both cohorts showed an increasing trend in incidence, which was confirmed by its peak in March 2024.
Fig. 1. Measles incidence rates (per 100,000 population) in Moscow in 2012–2023 among adults and children. The red dotted line shows the trend in incidence among the child population, and the black dotted line shows the trend in incidence among adults.
Рис. 1. Показатели заболеваемость корью (на 100 тыс. населения) в Москве в период с 2012 по 2023 г. среди взрослых и детей. Красная пунктирная линия отображает тренд среди детского населения, а черная пунктирная линия – тренд заболеваемости взрослых.
In connection with the COVID-19 pandemic in Moscow, a wide range of nonspecific prophylaxis and anti-epidemic measures were used, most of which were aimed at interrupting aerosol and contact transmission mechanisms [9–11]. Given the commonality of these transmission mechanisms for many diseases, it can be stated that the implementation of restrictive and quarantine measures had a positive effect on the reduction of the prevalence of all airborne infections. However, the registered decline in measles incidence in 2020–2021 is not indicative and most likely does not reflect the true characteristics of the epidemic process, because during the pandemic period there was a lacking diagnosis of infectious diseases associated with the overload of the health care system.
In Moscow, 2023 was characterized by an increase in measles incidence rates among both children (54.9 per 100,000 population) and adults (9.5 per 100,000 population), and the risk of getting sick with measles infection in children was 5.5 times higher than in adults (Fig. 1). Apparently, such a surge in measles incidence is associated with the cancellation of quarantine measures, the accumulation of unvaccinated persons due to the reduced activity of vaccination campaigns during the pandemic, unjustified medical withdrawals, as well as a large influx of labor migrants from neighboring countries with unknown vaccination history9. Furthermore, against the background of the COVID-19 pandemic, anti-vaccine sentiments have intensified worldwide, including in Russia [4].
The age structure of measles cases in children and adults during the study period was heterogeneous. Thus, in 2013, the ratio of the shares of children from 0 to 17 years of age and adults who became ill was 34.3% vs. 65.7%, and in 2017 – 66.4% vs. 33.6%, respectively (Fig. 2). In 2023, no statistically significant differences were found between the proportion of sick children and adults (53.8% and 46.2%). According to official statistics, the WHO targets for coverage of the country’s population with preventive vaccinations against measles have been successfully achieved and maintained at the level of at least 90% of the adult population and 95% of the child population6. At the same time, measles morbidity is determined by unvaccinated persons. It was noted that 92.5% (n = 2076) of all reported measles cases either did not have information on vaccination or were not reliably vaccinated in accordance with the national immunization schedule9.
Fig. 2. Proportion of adults among measles patients in Moscow in 2012–2023.
Рис. 2. Доли взрослых среди заболевших корью в г. Москве в 2012–2023 гг.
Unlike measles, the dynamics of rubella morbidity in Moscow until 2016 had a steady downward trend, which can be described by an exponential trend, and in recent years the incidence rate has remained at the same level – 0.02 per 100,000 population (Fig. 3), which is due to the improvement of epidemiological surveillance and control of this infection. At the same time, due to the high incidence of rubella in the late 1990s and early 2000s, the proportion of the population with post-infection immunity, which is more pronounced and persistent compared to post-vaccination immunity, remains in the population [12]. It should also be taken into account that a lower level of immunity is sufficient to limit the spread of rubella than measles, which is associated with a lower reproduction number for this infection.
Fig. 3. Rubella incidence rates (per 100,000 population) in Moscow in 2012–2023. The black dotted line shows the logarithmic trend line.
Рис. 3. Показатели заболеваемость краснухой (на 100 тыс. населения) в Москве в период с 2012 по 2023 г. Черным пунктиром показана логарифмическая линия тренда.
The incidence of mumps in Moscow has a stable sporadic character, but during the pandemic period caused by coronavirus infection, there was also a decrease in the number of registered cases of infection, which may have been caused by insufficient statistical recording of the diseased. In 2023, an increase in the incidence of epidemic mumps (67 cases; incidence rate 0.53 per 100,000 population) was observed in Moscow, which is 2.7 times higher than in 2022 (25 cases; incidence rate 0.20 per 100,000 population) and 2.9 times higher than in 2021 (23 cases; incidence rate 0.18 per 100,000 population)9.
Despite the importance of official statistics on incidence and documented immunization, they do not answer the main question: what is the actual protection of different age and social groups of the population against a particular infection? Due to possible violations of immunization schemes, lack of cold chain compliance during transportation and storage of vaccines, the presence in the population of persons who are not capable of producing a full immune response (non-responders), and other reasons [5, 7, 13–15], an objective assessment of the effectiveness of mass vaccination can be obtained only on the basis of serological data. Dynamic monitoring for the state of immunity of the population to infections controlled by means of specific prophylaxis makes it possible to timely identify signs of epidemiological disadvantage, indicating the beginning of the intensification of the epidemic process. Forecast of further development of the situation for each of the observed infections is considered unsatisfactory if there is a tendency to increase the proportion of seronegative persons and exceed its permissible level [8].
In order to ensure herd immunity against measles, rubella, mumps sufficient to prevent the spread of infection among the population, the immunization coverage of the population in the territory of the municipality should be as follows:
- vaccination and revaccination of at least 95% of children at the decreed ages against measles, rubella, mumps;
- at least 90% of women 18–25 years of age are immunized against rubella;
- at least 90% of adults 18–35 years of age are immunized against measles;
- no less than 90% of persons in decreed professions 18–55 years of age are immunized against measles10.
The relevance of population studies of various aspects of infectious pathology became the basis for the formation of a passport-verified collection of blood serum samples in the N.F. Gamaleya NRCEM. The use of the materials of the blood serum bank allows for large-scale scientific studies that significantly expand the understanding of the peculiarities of epidemiological processes of many infections [16–19]. In the framework of this study, serologic examination of more than 7000 blood serum samples obtained in 2019 from the conditionally healthy population living in Moscow and the Moscow region for the presence of specific antibodies to measles, rubella, and mumps viruses was performed. The choice of the time point was due to the fact that 2019 was the year preceding the beginning of the coronavirus pandemic and was also characterized by the maximum incidence of measles. In assessing the level of immunity, the subjects were stratified into age groups: 0–1 years, 2–5 years, 6–10 years and further in 5-year increments up to 60 years, 60–70 years and over 71 years of age. According to the questionnaires, data on presence/absence of vaccination were reported by 6829 individuals (91.6%), and data on the presence or absence of the history of disease were known for 6833 individuals (91.6%).
Since the study used questionnaire data to collect vaccination and infection history, not always the corresponding antibodies were detected in the serologic reactions of the examined persons who had information about encounters with measles, rubella or mumps pathogens (Fig. 4). The presence of data on the vaccine series and date of vaccination, as well as on the diagnosis of the disease and date of its diagnosis, is a reliable confirmation of vaccination and infection history. However, medical records with this information are not always available to the public. Nevertheless, data collection through questionnaires makes it possible to clarify the attitude of those surveyed to vaccination and indirectly estimate vaccination coverage in addition to official statistics.
Fig. 4. The proportion of seropositive persons to measles (a), rubella (b), mumps (c), depending on the vaccination status according to the questionnaire data in various age groups surveyed in 2019.
Рис. 4. Доля серопозитивных лиц к кори (а), краснухе (б), ЭП (в) в зависимости от вакцинального статуса согласно анкетным данным в разных возрастных группах лиц, обследованных в 2019 г.
Among those participants who reported a history of measles vaccination, 72.1% (95% CI 70.58–73.59%) had antibodies, and among those who did not indicate their vaccination status (i.e., did not have reliable information about it or did not wish to respond), 63.5% (95% CI 61.88–65.1%) had antibodies. Questionnaire data were most consistent with serologic findings in the 16–20 age group. Thus, 86.8% (95% CI 83.69–89.62%) of volunteers in this group who reported a history of measles had antibodies to the pathogen, while only 65.7% (95% CI 64.53–66.86%) of those who did not report the disease. A moderate correlation between vaccine history and antibody presence was found in the group of younger individuals (under 31 years of age) (Ka = 0.345, p < 0.001), and a weak correlation was found between antibody presence and information on past infection (Ka = 0.224, p < 0.001). In the group of individuals older than 31 years of age, there was a significant association between knowledge of past infection and antibody presence (Ka = 0.558, p < 0.001). No statistically significant association was found between vaccination history and antibody presence. According to the logistic regression model, parameters such as age, infection and vaccination history explained only 9.1% of the antibody presence data (Nagelkerke’s R2 = 0.091, p < 0.001). Data on past infection appear to be poorly informative for predicting the level of immunity to measles. A similar situation was observed for rubella and mumps. According to the logistic regression model, parameters such as age, history and vaccination history explained only 11.0% of the data for antibodies to rubella virus (Nagelkerke’s R2 = 0.110, p < 0.001) and 6.5% for mumps virus (Nagelkerke’s R2 = 0.065, p < 0.001).
With increasing age, there is a convergence of the graphs of the proportion of seropositive individuals, which can be explained either by an increase in the proportion of incorrect information about the vaccination performed, or by the history of infection, including asymptomatic form.
Analysis of the vaccination history of the surveyed persons with regard to measles showed that among children, 33 to 41% of respondents considered themselves unvaccinated (at the same time, for children under 14 years of age, in accordance with the conditions of participation in the study, the questionnaires were filled out by their parents or guardians). Among adults, the share of such persons was higher and reached 58% in the group of 56–60 years old. It should be noted that the above age group and persons older than this age were born before the start of mass vaccine prophylaxis in the 60s, which explains the obtained data on vaccine history. With regard to rubella and mumps, a comparable proportion of the surveyed persons considered themselves unvaccinated (no statistically significant differences were found, p > 0.05) (Table).
Table. Distribution of persons with different vaccination history (based on the survey) in the age groups of the examined persons
Таблица. Распределение лиц с разным вакцинальным анамнезом (на основе опроса) в возрастных группах обследованных лиц
Age group, years Возрастная группа, лет | Vaccination status (based on the survey: vaccinated – «+»; not vaccinated – «−») Вакцинальный статус (на основе опроса: привит – «+»; не привит – «−») | Measles Корь | Rubella Краснуха | Mumps Эпидемический паротит | |||
abs. абс. | % (95% CI / ДИ) | abs. абс. | % (95% CI / ДИ) | abs. абс. | % (95% CI / ДИ) | ||
0–1 | – | 15 | 39.47 (25.17–55.32) | 17 | 44.74 (29.8–60.44) | 19 | 50 (34.59–65.41%) |
+ | 23 | 60.53 (44.68–74.83) | 21 | 55.26 (39.56–70.2) | 19 | 50.00 (34.59–65.41) | |
2–5 | – | 68 | 33.01 (26.86–39.63) | 78 | 37.86 (31.45–44.62) | 77 | 38.89 (32.30–45.80) |
+ | 138 | 66.99 (60.37–73.14) | 128 | 62.14 (55.38–68.55) | 121 | 61.11 (54.20–67.70) | |
6–10 | – | 80 | 34.04 (28.21–40.27) | 87 | 37.02 (31.04–43.32) | 101 | 43.53 (37.27–49.96) |
+ | 155 | 65.96 (59.73–71.79) | 148 | 62.98 (56.68–68.96) | 131 | 56.47 (50.04–62.73) | |
11–15 | – | 69 | 41.82 (34.49–49.43) | 78 | 47.27 (39.76–54.88) | 88 | 54.66 (46.94–62.21) |
+ | 96 | 58.18 (50.57–65.51) | 87 | 52.73 (45.12–60.24) | 73 | 45.34 (37.79–53.06) | |
16–20 | – | 114 | 43.68 (37.76–49.74) | 168 | 64.37 (58.42–69.99) | 181 | 74.79 (69.05–79.95) |
+ | 147 | 56.32 (50.26–62.24) | 93 | 35.63 (30.01–41.58) | 61 | 25.21 (20.05–30.95) | |
21–25 | – | 367 | 44.00 (40.66–47.39) | 496 | 59.47 (56.11–62.77) | 600 | 76.24 (73.17–79.11) |
+ | 467 | 56.00 (52.61–59.34) | 338 | 40.53 (37.23–43.89) | 187 | 23.76 (20.89–26.83) | |
26–30 | – | 633 | 50.36 (47.60–53.12) | 817 | 65.00 (62.33–67.60) | 919 | 77.75 (75.31–80.05) |
+ | 624 | 49.64 (46.88–52.40) | 440 | 35.00 (32.40–37.67) | 263 | 22.25 (19.95–24.69) | |
31–35 | – | 773 | 54.47 (51.88–57.05) | 946 | 66.67 (64.18–69.08) | 1044 | 77.68 (75.39–79.84) |
+ | 646 | 45.53 (42.95–48.12) | 473 | 33.33 (30.92–35.82) | 300 | 22.32 (20.16–24.61) | |
36–40 | – | 506 | 53.89 (50.69–57.06) | 659 | 70.18 (67.20–73.04) | 705 | 79.30 (76.55–81.87) |
+ | 433 | 46.11 (42.94–49.31) | 279 | 29.74 (26.88–32.73) | 184 | 20.70 (18.13–23.45) | |
41–45 | – | 297 | 53.80 (49.63–57.93) | 402 | 72.83 (69.00–76.41) | 437 | 82.14 (78.72–85.22) |
+ | 255 | 46.20 (42.07–50.37) | 150 | 27.17 (23.59–31.00) | 95 | 17.86 (14.78–21.28) | |
46–50 | – | 154 | 50.33 (44.74–55.90) | 228 | 74.51 (69.41–79.15) | 241 | 81.97 (77.28–86.04) |
+ | 152 | 49.67 (44.10–55.26) | 78 | 25.49 (20.85–30.59) | 53 | 18.03 (13.96–22.72) | |
51–55 | – | 127 | 55.46 (48.99–61.79) | 179 | 78.17 (72.48–83.14) | 185 | 83.71 (78.42–88.13) |
+ | 102 | 44.54 (38.21–51.01) | 50 | 21.83 (16.86–27.52) | 36 | 16.29 (11.87–21.58) | |
56–60 | – | 111 | 58.73 (51.62–65.57) | 147 | 77.78 (71.46–83.25) | 150 | 82.87 (76.89–87.82) |
+ | 78 | 41.27 (34.43–48.38) | 42 | 22.22 (16.75–28.54) | 31 | 17.13 (12.18–23.11) | |
61–70 | – | 95 | 55.56 (48.07–62.86) | 140 | 81.87 (75.59–87.09) | 149 | 88.17 (82.66–92.38) |
+ | 76 | 44.44 (37.14–51.93) | 31 | 18.13 (12.91–24.41) | 20 | 11.83 (7.62–17.34) | |
71 and older 71 и старше | – | 18 | 64.29 (45.84–79.94) | 25 | 89.29 (74.09–96.89) | 25 | 89.29 (74.09–96.89) |
+ | 10 | 35.71 (20.06–54.16) | 3 | 10.71 (3.11–25.91) | 3 | 10.71 (3.11–25.91) | |
Total Итого | – | 3427 | 50.18 (49.00–51.37) | 4467 | 65.42 (64.29–66.54) | 4921 | 75.73 (74.68–76.76) |
+ | 3402 | 49.82 (49.63–51.00) | 2361 | 34.58 (33.46–35.71) | 1577 | 24.27 (23.24–25.32) | |
There were differences in the distribution of individuals seropositive to the studied infections in different age groups. On average, 67.38% (95% CI 66.31–68.44%) of subjects were immune to measles virus, 90.65% (95% CI 89.98–91.3%) to rubella virus, and 75.25% (95% CI 74.24–76.24%) to mumps (Fig. 5). At the same time, the proportion of persons immune to all three infections was lowest in the age group up to 24 months and did not exceed 50% of those examined, which can be explained by vaccination against the three infections under study at the age of 12 months. It is likely that not all children in this age group had received the appropriate vaccine at the time of the study.
Fig. 5. Distribution of persons seropositive to measles, rubella, and mumps viruses among different age groups surveyed in 2019.
Рис. 5. Распределение серопозитивных лиц к вирусам кори, краснухи и ЭП среди разных возрастных групп, обследованных в 2019 г.
Nevertheless, in the age group 6–10 years, more than 90% of children should have received at least one dose of vaccine according to official statistical reporting on vaccination coverage in the decreed age groups. According to the data obtained, only 61.34% (95% CI 55.46–67.06%) of the examined individuals in this age group had specific IgG antibodies. The proportions immune to mumps and rubella viruses were 68.05% (95% CI 62.33–73.5%) and 76.58% (95% CI 71.34–81.44%), respectively.
Of note is the decreased rate of increase in the proportion of seropositive individuals in the group 31 to 35 years of age (31 years to 40 years of age in the case of mumps). Only 63.26% (95% CI 60.84–65.66%), 88.69% (95% CI 87.05–90.22%) and 70.85% (95% CI 68.49–73.15%) were immune, respectively.
Among those under 50 years of age, the proportion of persons immune to the three infections under study was similar, with the lowest proportion immune to measles and the highest to rubella. Above this age, the situation began to change somewhat – measles and rubella had almost the same proportion of immune persons, approaching 100%, while the proportion of immune persons to mumps was lower and reached 90% only in the oldest age group.
Discussion
The analysis of the epidemiological situation of measles, rubella and mumps in Moscow from 2012 to 2023 has allowed to establish the presence of multidirectional trends, despite the fact that all these infections are included in a single unified system of epidemiological surveillance, and effective attenuated vaccines of stable antigenic composition administered to children at the age of 12 months and 6 years are used for their prevention. Furthermore, according to official statistical reports, vaccination coverage for the three infections is more than 90% among adults and 95% among children. However, the epidemic process of these infections to date is different and is objectively manifested by a wave-like increase in measles incidence, stabilization of rubella case registration at a sporadic level and unstable incidence of mumps with a slight tendency to increase over the last 3 years9. The results of serologic studies of the prevalence of specific IgG antibodies in different age groups of the population of Moscow city and Moscow region among persons with different vaccination and infection history corresponded to the age structure of incidence for each of the three infections under study.
It should be taken into account that the vaccination and infection history collected from the words of the examined persons, without documentary confirmation, has limited scientific significance and in older age groups may be unreliable due to natural reasons. Nevertheless, in pediatric and young adult populations, its collection is preferable, as information on the encounter with the pathogen is stored in modern electronic medical records and vaccination certificates, which are available for review by the persons involved in the study. It is important that up to 40% of the surveyed children were not immunized, according to their legal representatives, which can largely explain the identified significant proportions of non-immunized persons among them and indicates a high prevalence of anti-vaccination beliefs among the population [2, 5, 6]. In the survey of the child population, vaccination of which is a significant issue for their legal representatives who filled in the questionnaire of our study, it was shown that anamnestic data have the greatest reliability (confirmed serologically) and can indirectly be used to estimate vaccination coverage. Taking into account the fact that the timing of vaccine administration for the prevention of all three infections under study is the same, combined vaccines have been developed and are available for use, the differences in the proportion of persons immune to pathogens can be explained by the different immunologic efficacy of the respective vaccines. In age groups older than 56 years, vaccine history was not of high value for the study, since herd immunity in them is determined by childhood infection, when the prevalence of measles, rubella, and mumps was many times higher than today, and mass vaccination was not carried out. Furthermore, serologic data in this age group illustrate that the persistence of IgG antibodies after measles and rubella infection practically does not differ and is close to 100%.
It is shown that the formed high level of herd immunity to rubella virus currently prevents the spread of infection among the population. These data are consistent with our earlier results on the assessment of immunologic susceptibility of the metropolitan population [7]. At the same time, it should be noted that the contribution of vaccination to the formation of population immunity is limited to the pediatric population, while adults were born before the mass application of the vaccine and are immune due to the transferred infection.
With regard to mumps, the epidemic situation is relatively favorable, but the formed level of herd immunity does not allow to reduce the incidence to a stable sporadic level. It was found that among the child population under 16 years of age, the proportion of immune persons in 2019 was less than 80%, obviously this contributes to the accumulation of non-immune persons in the population and threatens, if this trend continues, to manifest itself in a further increase in morbidity. This is also confirmed by the data of epidemiologic analysis on a slight increase in incidence in 2021–2023. The results obtained indicate the need to carry out preventive measures for vaccination of the population not covered earlier.
The observed trend of measles incidence growth in the last decade can be explained by the accumulation of non-immune individuals among young and child population, which is convincingly shown by the results of the study. The unfavorable trend towards an increase in the proportion of seronegative individuals among different population groups has been shown by many authors who have screened the prevalence of specific IgG antibodies in Russia and Europe [3, 20–23]. The obtained data of the serologic study on the presence of a significant proportion of non-immune individuals among children and young adults in 2019 indicate a high risk of increased incidence in the future. Thus, among the examined children, the proportion of seropositive individuals was maximum in the groups of children 6–10 and 11–15 years of age and amounted to only 61.3%. This risk was realized at the end of the COVID-19 pandemic in 2023, when in Moscow the measles incidence rates among both children (54.9 per 100,000 population) and adults (9.5 per 100,000 population) exceeded the values of 2019 (25.9 and 11.1 per 100,000 population, respectively) and became the highest for the study period from 2012 to 2023. At the same time, the risk of getting measles in children was 5.5 times higher than in adults.
Similar alarming data are confirmed by foreign experts who note slow recovery rates of coverage of routine vaccinations against measles, rubella and other vaccine-preventable infections as a result of the COVID-19 pandemic. According to WHO and UNICEF, the incidence in the European Region continues to grow and the number of measles cases reported in 2024 will soon exceed the total for the entirety of 20231112.
Conclusion
Based on the results of this study, the significance of serologic studies for determining the risks of infectious disease spread among the population has been convincingly demonstrated. It was shown that the level of herd immunity to rubella (90.65% (95% CI 89.98–91.3%)) allows to practically stop the spread of this infection. With regard to mumps, 75.25% (95% CI 74.24–76.24%) of the examined persons were immune, which seems to be a condition for the observed decrease in the incidence of the disease in the territory of Moscow. Nevertheless, there is a risk of accumulation of the proportion of non-immune individuals in the future, which is fraught with an increase in case registration. The current unfavorable epidemiological situation with measles is largely determined by the presence of cohorts of non-immune persons among children and young adults (the share of immune persons was about 60%), which is manifested by the maximum incidence rates in these groups among the entire population. The currently formed level of herd immunity does not allow preventing the wave-like increase in incidence registered in recent years.
Due to active migration processes in the metropolitan area, as well as difficulties in achieving the target levels of vaccination coverage during the COVID-19 pandemic, it is necessary to adjust the vaccine prophylaxis tactics and to carry out measures for mopping up and catch-up immunization of the population with regard to measles and mumps, especially in the age groups at risk.
1 50th anniversary of the Expanded Programme on Immunization (EPI); 2024. Available at: https://who.int/news-room/events/detail/2024/01/01/default-calendar/50th-anniversary-of-the-expanded-programme-on-immunization-(epi)
2 Global immunization efforts have saved at least 154 million lives over the past 50 years; 2024. Available at: https://www.unicef.org/eca/press-releases/global-immunization-efforts-have-saved-least-154-million-lives-over-past-50-years
3 Eliminating measles and rubella and preventing congenital rubella infection. WHO European Region strategic plan, 2005–2010. Available at: https://who-sandbox.squiz.cloud/__data/assets/pdf_file/0008/79028/E87772.pdf
4 WHO. European Vaccine Action Plan 2015–2020. Copenhagen; 2014. Available at: https://apps.who.int/iris/handle/10665/340400
5 WHO. The European Immunization Agenda 2030. Copenhagen; 2021. Available at: https://who.int/europe/initiatives/the-european-immunization-agenda-2030
6 State Report «On the state of sanitary and epidemiological welfare of the population in the Russian Federation in 2023». Moscow; 2024.
7 WHO. Measles and rubella monthly update – WHO European Region – July 2024; 2024. Available at: https://who.int/europe/publications/m/item/measles-and-rubella-monthly-update---who-european-region---july-2024
8 MU 3.1.2943–11. Organization and conduct of serological monitoring of the state of collective immunity to infections controlled by means of specific prevention (diphtheria, tetanus, whooping cough, measles, rubella, mumps, polio, hepatitis B). Moscow; 2011.
9 State report «On the state of sanitary and epidemiological welfare of the population in the city of Moscow in 2023». Moscow; 2024.
10 SanPiN 3.3686–21. Sanitary and epidemiological requirements for the prevention of infectious diseases. Мoscow; 2021.
11 UNICEF. Measles cases across Europe continue to surge, putting millions of children at risk; 2024. Available at: https://unicef.org/press-releases/measles-cases-across-europe-continue-surge-putting-millions-children-risk
12 WHO. Rapid response to measles outbreak is critical, as cases this year predicted to soon exceed total number reported in 2023; 2024. Available at: https://who.int/europe/news/item/28-05-2024-joint-press-release-from-who-and-unicef--measles-cases-across-europe-continue-to-surge--putting-millions-of-children-at-risk
About the authors
Yana V. Simakova
National Research Centre for Epidemiology and Microbiology Named After Honorary Academician N. F. Gamaleya of the Ministry of Health of the Russian Federation
Email: y.v.simakova@yandex.ru
ORCID iD: 0000-0002-5033-6931
Researcher
Russian Federation, 123098, MoscowVladimir A. Gushchin
National Research Centre for Epidemiology and Microbiology Named After Honorary Academician N. F. Gamaleya of the Ministry of Health of the Russian Federation; I.M. Sechenov First Moscow State Medical University of the Ministry of Health of the Russian Federation (Sechenov University); Lomonosov Moscow State University
Author for correspondence.
Email: wowaniada@yandex.ru
ORCID iD: 0000-0002-9397-3762
Doctor of Biological Sciences, Associate Professor, Leading researcher, Head of the Department, Head of the Department of Medical Genetics, Senior Researcher at the Department of Virology, Faculty of Biology
Russian Federation, 123098, Moscow; 119048, Moscow; 119234, MoscowTatiana A. Semenenko
National Research Centre for Epidemiology and Microbiology Named After Honorary Academician N. F. Gamaleya of the Ministry of Health of the Russian Federation; I.M. Sechenov First Moscow State Medical University of the Ministry of Health of the Russian Federation (Sechenov University)
Email: semenenko@gamaleya.org
ORCID iD: 0000-0002-6686-9011
Doctor of Medical Sciences, Professor, Chief Researcher
Russian Federation, 123098, Moscow; 119048, MoscowDaria A. Ogarkova
National Research Centre for Epidemiology and Microbiology Named After Honorary Academician N. F. Gamaleya of the Ministry of Health of the Russian Federation
Email: DashaDv1993@gmail.com
ORCID iD: 0000-0002-1152-4120
Junior Researcher
Russian Federation, 123098, MoscowDenis A. Kleymenov
National Research Centre for Epidemiology and Microbiology Named After Honorary Academician N. F. Gamaleya of the Ministry of Health of the Russian Federation
Email: mne10000let@yandex.ru
ORCID iD: 0000-0001-9422-7238
PhD, Senior Researcher, Head of the Laboratory
Russian Federation, 123098, MoscowAnna V. Nozdracheva
National Research Centre for Epidemiology and Microbiology Named After Honorary Academician N. F. Gamaleya of the Ministry of Health of the Russian Federation
Email: nozdrachevaav@gamaleya.org
ORCID iD: 0000-0002-8521-1741
Ph.D., Senior Researcher, Head of the Laboratory
Russian Federation, 123098, MoscowVictor A. Manuylov
National Research Centre for Epidemiology and Microbiology Named After Honorary Academician N. F. Gamaleya of the Ministry of Health of the Russian Federation; Novosibirsk State University
Email: victormanuilov@yandex.com
ORCID iD: 0000-0002-2296-6151
PhD, Senior Researcher, Faculty of Natural Sciences
Russian Federation, 123098, Moscow; 630090, NovosibirskArtem P. Tkachuk
National Medical Research Center for Phthisiopulmonology and Infectious Diseases of the Ministry of Health of the Russian Federation
Email: artem.p.tkachuk@gmail.com
ORCID iD: 0000-0003-3262-4873
PhD, Leading Researcher
Russian Federation, 127994, MoscowAlexander L. Gintsburg
National Research Centre for Epidemiology and Microbiology Named After Honorary Academician N. F. Gamaleya of the Ministry of Health of the Russian Federation; I.M. Sechenov First Moscow State Medical University of the Ministry of Health of the Russian Federation (Sechenov University)
Email: gintsburg@gamaleya.org
ORCID iD: 0000-0003-1769-5059
Doctor of Biological Sciences, Professor, Academician of the Russian Academy of Sciences, Director, Head of the Department of Infectology
Russian Federation, 123098, Moscow; 119048, MoscowReferences
- Tatochenko V.K., Ozeretskovsky N.A. Immunoprophylaxis 2020 (Reference Book). Epidemiologiya i vaktsinoprofilaktika. 2020; 19(6): 100. https://elibrary.ru/uhbxbs (in Russian)
- Semenenko T.A., Smetanina S.V., Kolobukhina L.V., Karetkina G.N., Nozdracheva A.V., Kruzhkova I.S., et al. Measles: epidemiological features during the elimination period, modern possibilities of prevention, diagnosis and treatment. the importance of a serological study of the population immunity of the population. Methodological recommendations No. 74. Moscow; 2020. (in Russian)
- Tsvirkun O.V., Tikhonova N.T., Turaeva N.V., Ezhlova E.B., Melnikova A.A., Gerasimova A.G., et al. Population immunity and structure of measles cases in the Russian Federation. Epidemiologiya i vaktsinoprofilaktika. 2020; 19(4): 6–13. https://doi.org/10.31631/2073-3046-2020-19-4-6-13 https://elibrary.ru/phmiue (in Russian)
- Semenenko T.A., Nozdracheva A.V. Analysis and outlook for the development of measles epidemic situation during the COVID-19 pandemic. Epidemiologiya i vaktsinoprofilaktika. 2021; 20(5): 21–31. https://doi.org/10.31631/2073-3046-2021-20-5-21-31 https://elibrary.ru/jjvvwf (in Russian)
- Chernova T.M., Timchenko V.N., Myskina N.A., Lapina M.A., Orekhova A.E., Kanina A.D. Causes of violation of vaccination schedule in young children. Pediatr. 2019; 10(3): 31–6. https://doi.org/10.17816/PED10331-36 https://elibrary.ru/facwbw (in Russian)
- Moiseeva K.E., Alekseeva A.V. Main reasons for vaccination refusals. Sotsial’nye aspekty zdorov’ya naseleniya. 2019; 65(5): 9. https://doi.org/10.21045/2071-5021-2019-65-5-9 https://elibrary.ru/aywtkt (in Russian)
- Nozdracheva A.V., Asatryan M.N., Asatryan M.N., Shmyr I.S., Ershov I.F., Solov’ev D.V., et al. Immunological susceptibility of metropolis population to measles in its elimination stage. Epidemiologiya i vaktsinoprofilaktika. 2019; 18(2): 18–26. https://doi.org/10.31631/2073-3046-2019-18-2-18-26 (in Russian)
- Semenenko Т.А., Akimkin V.G. Seroepidemiology in the surveillance of vaccine-preventable diseases. Journal of Microbiology, Epidemiology and Immunobiology. 2018; 95(2): 87–94. https://doi.org/10.36233/0372-9311-2018-2-87-94 https://elibrary.ru/yxuagt (in Russian)
- Semenenko T.A. Epidemiological aspects of non-specific prevention of infectious diseases. Vestnik Rossiiskoi akademii meditsinskikh nauk. 2001; 56(11): 25–9. (in Russian)
- Akimkin V.G., Semenenko T.A., Ugleva S.V., Dubodelov D.V., Kuzin S.N., Yatsyshina S.B., et al. COVID-19 in Russia: epidemiology and molecular genetic monitoring. Vestnik Rossiiskoi akademii meditsinskikh nauk. 2022; 77(4): 254–60. https://doi.org/10.15690/vramn2121 https://elibrary.ru/dozijs (in Russian)
- Briko N.I., Kagramanyan I.N., Nikiforov V.V., Suranova T.G., Chernyavskaya O.P., Polezhaeva N.A. COVID-19. Prevention measures in the Russian Federation. Epidemiologiya i vaktsinoprofilaktika. 2020; 19(2): 4–12. https://doi.org/10.31631/2073-3046-2020-19-2-4-12 https://elibrary.ru/ruwkxq (in Russian)
- Pozdnyakov A.A., Chernyavskaya O.P. Manifestations of the epidemic process of measles and Rubella at the present stage. Epidemiologiya i vaktsinoprofilaktika. 2018; 17(5): 45–53. https://doi.org/10.31631/2073-3046-2018-17-5-45-53 https://elibrary.ru/vouvre (in Russian)
- Nozdracheva A.V., Asatryan M.N., Rybak L.A., Voloshkin A.A., Semenenko A.V. Improvement of epidemiological diagnosis in the system of epidemiological surveillance of current infections by creating a database of the results of foci investigation. Sanitarnyi vrach. 2022; (5): 316–25. https://doi.org/10.33920/med-08-2205-01 https://elibrary.ru/mjqfsh (in Russian)
- Semenenko Т.A. Immune response after vaccination against hepatitis B in patients with immunodeficiency. Epidemiologiya i vaktsinoprofilaktika. 2011; (1): 51–8. https://elibrary.ru/ndihiz (in Russian)
- Zhukova E.V., Mirskaya M.A., Gotvyanskaya T.P., Kaira A.N., Semenenko A.V., Nozdracheva A.V., et al. On the issue of the safety of domestic vaccines against new coronavirus infection in medical workers. Sanitarnyi vrach. 2024; (2): 92–104. https://doi.org/10.33920/med-08-2402-01 https://elibrary.ru/isrlfo (in Russian)
- Semenenko T.A. The role of the blood serum bank in the biological safety system of the country. Vestnik Roszdravnadzora. 2010; (3): 55–8. https://elibrary.ru/muutej (in Russian)
- Gushchin V.A., Manuilov V.A., Mazunina E.P., Kleymenov D.A., Semenenko T.A., Gintsburg A.L., et al. Immunological memory as a basis for a wise vaccination strategy. A rationale for introducing a comprehensive seroepidemiological surveillance system in Russia. Bulletin of Russian State Medical University. 2017; (5): 5–25. https://doi.org/10.24075/brsmu.2017-05-01 https://elibrary.ru/zwrdtx
- Semenenko T.A., Ananyina Yu.V., Boev B.V., Ginzburg A.L. Banks of biological resources in the system of fundamental epidemiological and clinical research. Vestnik Rossiiskoi akademii meditsinskikh nauk. 2011; 66(10): 5–9. https://elibrary.ru/oghqpb (in Russian)
- Anisimov S.V., Meshkov A.N., Glotov A.S., Borisova A.L., Balanovsky O.P., Belyaev V.E., et al. National association of biobanks and biobanking specialists: new community for promoting biobanking ideas and projects in Russia. Biopreserv. Biobank. 2021; 19(1): 73–82. https://doi.org/10.1089/bio.2020.0049
- Nozdracheva A.V., Semenenko T.A. The status of herd immunity to measles in Russia: A systematic review and meta-analysis of epidemiological studies. Zhurnal mikrobiologii, epidemiologii i immunobiologii. 2020; 97(5): 445–57. https://doi.org/10.36233/0372-9311-2020-97-5-7 https://elibrary.ru/cquubm (in Russian)
- Böröcz K., Samardžić S., Drenjančević I., Markovics Á., Berki T., Németh P. Dynamic features of herd immunity: similarities in age-specific anti-measles seroprevalence data between two countries of different epidemiological history. J. Clin. Med. 2022; 11(4): 1145. https://doi.org/10.3390/jcm11041145
- Plans-Rubió P. Low percentages of measles vaccination coverage with two doses of vaccine and low herd immunity levels explain measles incidence and persistence of measles in the European Union in 2017–2018. Eur. J. Clin. Microbiol. Infect. Dis. 2019; 38(9): 1719–29. https://doi.org/10.1007/s10096-019-03604-0
- Semenenko T.A., Nozdracheva A.V., Asatryan M.N., Akimkin V.G., Tutelyan A.V., Shmyr I.S., et al. Multivariate analysis of the megacity population immunity to measles. Vestnik Rossiiskoi akademii meditsinskikh nauk. 2019; 74(5): 351–60. https://doi.org/10.15690/vramn1170 https://elibrary.ru/wwtsug (in Russian)
Supplementary files