Частота выявления антител класса IgG к вирусу Mpox и осведомленность о заболевании Mpox в Ибадане, юго-западная Нигерия
- Авторы: Olayiwola J.1, Akagbosu A.1, Samson O.1, Alaba A.1, Aponjolosun B.1, Soyemi S.2
-
Учреждения:
- Университет Аджайи Кроутер
- Больница университетского колледжа, Ибадан
- Выпуск: Том 70, № 5 (2025)
- Страницы: 463-470
- Раздел: ОРИГИНАЛЬНЫЕ ИССЛЕДОВАНИЯ
- URL: https://virusjour.crie.ru/jour/article/view/16793
- DOI: https://doi.org/10.36233/0507-4088-337
- EDN: https://elibrary.ru/spvndn
- ID: 16793
Цитировать
Полный текст
Аннотация
Цель. Ранее случаи Mpox были распространены среди детей; недавние вспышки, вызванные вирусом клады II, в основном затронули лиц молодого возраста. Исследование направлено на изучение знаний о вирусе Mpox и отношения к нему, а также серопревалентности среди когорты лиц в Ибадане, давших согласие на участие в исследовании.
Материалы и методы. К участию в исследовании были допущены добровольцы, соответствовавшие установленным критериям включения. Было проведено поперечное исследование с участием 94 респондентов для изучения социально-демографических факторов, уровня осведомленности, отношения к профилактике и уровня инфицирования. Антитела класса IgG к вирусу Mpox количественно определяли с помощью метода твердофазного иммуноферментного анализа (ИФА). Затем данные анализировали с использованием критерия χ2, а количественное определение антител отображали с помощью диаграммы типа «ящик с усами»; статистическую значимость определяли при p < 0,05.
Результаты. Большинство респондентов были женщинами (66,7%) в возрасте 58 лет и старше (20,0%). Большинство имели высшее (40,0%) и среднее образование (34,4%). Осведомленность об Mpox была умеренной: 61,1% опрошенных слышали о вирусе в основном из новостей (20,0%) и от работников здравоохранения (18,9%). Тем не менее пробелы в знаниях были очевидны: только 38,9% знали о симптомах заболевания и 40,0% понимали пути передачи вируса. Отношение к профилактике было в целом положительным; 60,0% считали, что Mpox можно предотвратить, и 73,3% были готовы вакцинироваться. Тем не менее готовность участвовать в скрининге была низкой; 81,1% респондентов никогда не проходили тестирование, а 58,9% не знали о доступности теста в их регионе. Что касается серопревалентности, у женщин частота выявления анти-Mpox была значительно выше (27,4%), чем у мужчин (9,6%) (χ2 = 3,854, p = 0,050). В возрастном разрезе самые высокие показатели серопозитивности наблюдались у лиц младше 18 лет (61,5%) и в возрасте от 53 до 57 лет (66,6%) (χ2 = 30,817, p = 0,000), что указывает на значительные возрастные различия.
Заключение. Полученные данные подчеркивают необходимость целевого просвещения в области общественного здравоохранения, расширения доступа к тестированию и разработки стратегий целенаправленного вмешательства для улучшения профилактики и контроля Mpox, особенно среди уязвимых возрастных групп и малоинформированного населения.
Ключевые слова
Полный текст
Background
Monkeypox (Mpox) is a viral disease pathogen of which belongs to the Poxviridae family, a group of large and complex DNA viruses. It has been characterized into two groups of strains with varying case fatality rates [1]. Between January 1, 2022, and February 1, 2023, more than 87,000 cases and 141 deaths attributed to human Mpox were reported in 111 countries worldwide [2]. Since 1970, when it was first confirmed, monkeypox has been reported in central and western African countries, including Cameroon, the Central African Republic, the Democratic Republic of Congo, and Nigeria [3, 4]. However, the actual burden of monkeypox in Sub-Saharan Africa remains poorly defined.
The increased global spread of Mpox recently underscores the need for enhanced surveillance and public health emergency preparedness, especially in areas with weak health systems, such as Nigeria [5, 6]. The first occurrence of the disease outside Africa was in the USA in 2003, with 47 human cases attributed to close contact with prairie dogs believed to have been infected by rodents imported from Ghana [7]. Subsequently, four additional cases outside Africa were detected, linked to the largest clade II monkeypox virus (previously called West African clade) outbreak between 2017 and 2018 [3, 8]. The outbreaks of Mpox in Europe and North America suggest the potential for further transmission in non-endemic settings [9–11].
Additionally, most cases of Mpox in Nigeria do not report contact with animals, while over 50% have a history of contact with persons with similar skin lesions. The clade II monkeypox virus was previously described as causing a less severe illness than the Congo-basin clade and smallpox [7]. Nevertheless, some cases in Nigeria were associated with adverse outcomes [8, 12]. Consequently, further research is needed on the possible risk factors for mpox and its severity as observed in recent outbreaks, including the role of immunity and coinfections [9].
The discontinuation of routine smallpox vaccinations since 1980 and the potential for asymptomatic human-to-human transmission may have played a role in the virus’s evolution [13]. Additionally, changes in human behavior, travel patterns, and population movement have likely contributed to the rapid spread of the 2022 outbreak [11, 14]. Despite increasing case numbers, research on the epidemiology, clinical symptoms, and transmission pathways remains limited [15]. As the outbreak continues to evolve, further studies will be essential in improving our understanding of the virus and refining public health responses [15]. Therefore, this study was carried out to investigate the seroprevalence of anti-Mpox virus IgG antibody in Ibadan, Southwest Nigeria.
Materials and methods
Study Location and Design
This study was conducted at the Ibadan North Local Government, Oyo State, Nigeria, from January to June 2025. Eligible individuals were people who consented to participate, while ineligibility was due to non-consent. A cross-sectional and laboratory-based study was used to investigate the occurrence and prevalence of the virus. Institutional ethical approval (FNS/ERC/2024/025SM) to carry out this work was granted by the Research Ethics Committee of the Faculty of Natural Sciences, Ajayi Crowther University, Oyo State, Nigeria.
Demographic Data Collection
A structured questionnaire was used to assess the socio-demographic data of the participants, as well as their awareness, knowledge, and attitudes towards Mpox infection, after obtaining verbal consent following proper education of the participants.
Sample Collection
A total of 94 blood samples were collected from participants via venipuncture after obtaining their consent. The minimum sample size for estimating anti-Mpox IgG seroprevalence was computed using Cochran’s formula with 95% confidence (Z = 1.96), anticipated prevalence of 7% (Cochrane, 1977), and desired precision (d = 0.05), yielding a total of 100 samples. Allowing for an anticipated 10% non-response rate, the target sample size was 111 respondents. Ultimately, 94 participants were enrolled and included in the final analysis due to resource constraints. The blood samples were collected into the EDTA bottles and spun by centrifugation at 3000 rpm for 10 minutes to separate the serum. The serum is then separated into a plain bottle and kept at -80o C before the serological assay according to Reed et al. [2004].
The work was duly approved by the Research Ethics Committee of the Faculty of Natural Sciences, Ajayi Crowther University, Oyo. The approval number (FNS/ERC/2024/025SM) was given for the conduct of the research.
Detection of Anti-Mpox Virus IgG Antibody
This Mpox-IgG Antibody ELISA kit was used to detect the occurrence of anti-Mpox IgG antibody by measuring the intensity of the color change using a spectrophotometer. The standard curve was prepared by plotting Optical Density against the of anti-Mpox IgG antibody concentration obtained from standards according to the manufacturer and was therefore used for the interpretation of the readings from the sera.
Data analysis
Data collected was statistically analyzed to evaluate the association between different variables at 95% confidence intervals using SPSS version 23. Statistical value below 0.05 (p < 0.05) was considered statistically significant. A Box and Whisker plot was used to present the concentration of anti-Mpox virus IgG antibody. The data is then presented using frequency tables, simple ratios, percentages, and charts.
Results
Socio-demographic variables among the respondents
The socio-demographic data showed a variety of ages of the respondents, with ≥ 58 years having the highest occurrence (20.0%), while 23–27 years were the least age group (4.4%). There were more females (66.7%) among the respondents and males (23.3%); however, 10.0% of the respondents did not disclose their gender (Table 1).
Table 1. Socio-demographic variables among the respondents
Таблица 1. Социально-демографические данные респондентов
Demography / Демография | Frequency (%) / Частота (%) |
Age (years) / Возраст (годы) | |
< 18 18–22 23–27 28–32 33–37 38–42 43–47 47–52 53–57 58 above / 58 и более No response / Нет ответа | 14 (15.6) 6 (6.7) 4 (4.4) 2 (2.2) 10 (11.1) 5 (5.6) 9 (10.0) 10 (11.1) 4 (4.4) 18 (20.0) 8 (8.9) |
Gender / Пол | |
Male / Мужчины Female / Женщины No response / Нет ответа | 21 (23.3) 60 (66.7) 9 (10.0) |
Educational Level / Образование | |
No formal education / Нет образования Primary / Начальное Secondary / Среднее Tertiary / Высшее No response / Нет ответа | 1 (1.1) 10 (11.1) 31 (34.4) 36 (40.0) 12 (13.3) |
Ethnicity / Этническая принадлежность | |
Yoruba / йоруба Igbo / игбо Hausa / хауса No response / Нет данных | 35 (38.9) 39 (43.3) 1 (1.1) 15 (16.7) |
Religion / Религия | |
Christianity / Христианство Islamic / Ислам No response / Нет ответа | 77 (85.6) 3 (3.3) 10 (11.1) |
Awareness and Knowledge of the Mpox Virus among the Respondents
The knowledge of the Mpox disease, its symptoms, and transmission was observed among 55 (61.1%) respondents. The means of awareness about Mpox disease was observed to be more (20.0%) through broadcasting, while 18.9% of the respondents heard through healthcare workers; however, 34.4% of the respondents have not heard about Mpox infection (Table 2).
Table 2. Awareness and Knowledge of the Mpox Virus among the Respondents
Таблица 2. Осведомленность и знания о вирусе Mpox среди респондентов
Variables / Вопросы | Frequency (%) / Частота (%) |
Have you heard of the Mpox virus? Слышали ли вы о вирусе Mpox? | |
Yes / Да No / Нет No response / Нет ответа | 55 (61.1) 28 (31.1) 7 (7.8) |
If yes, what is your primary source of information about the Mpox virus? Если да, то какой у вас основной источник информации о вирусе Mpox? | |
News / Новости Social media / Соцсети Healthcare workers / Работники здравоохранения Friends/Family / Друзья/Семья Others / Другие No response / Нет ответа | 18 (20.0) 13 (14.4) 17 (18.9) 7 (7.8) 4 (4.4) 31 (34.4) |
Do you know the symptoms of the Mpox virus? Знаете ли вы симптомы инфекции, вызванной вирусом Mpox? | |
Yes / Да No / Нет No response / Нет ответа | 35 (38.9) 42 (46.7) 13 (14.4) |
If yes, which of these do you associate with Mpox virus? Если да, то какие из них вы связываете с вирусом Mpox? | |
Fever / Лихорадка Skin rashes / Кожная сыпь Headaches / Головная боль Muscle aches / Мышечные боли No response / Нет ответа | 15 (16.7) 18 (20.0) 7 (7.8) 4 (4.4) 46 (51.1) |
Do you know how the Mpox virus is transmitted? Знаете ли вы, как передается вирус Mpox? | |
Yes / Да No / Нет No response / Нет ответа | 36 (40.0) 44 (48.9) 10 (11.1) |
If yes, which of these do you think is a mode of transmission? Если да, то какой из перечисленных ниже, по вашему мнению, является путем передачи? | |
Direct contact with infected person / Прямой контакт с инфицированным человеком Contact with animals / Контакт с животными Airborne droplets / Воздушно-капельный путь Others / Другое No response / Нет ответа | 25 (27.8) 6 (6.7) 9 (10.0) 1 (1.1) 49 (54.4) |
Attitudes toward Mpox Virus Prevention among Respondents
There were 54 (60.0%) of the respondents who knew that Mpox disease can be prevented, while 24 (26.7%) did not believe Mpox disease can be prevented; however, 12 (13.3%) of respondents did not respond. It was observed that 16 (17.8%) of the respondents were ready for regular handwashing, while 9 (10.0%) of the respondents were ready to wear protective devices for prevention. There were 66 (73.3%) of the respondents who indicated willingness to take the Mpox virus vaccine, while 6 (6.7%) of the respondents expressed a phobia of the vaccine against Mpox disease (Table 3).
Table 3. Attitudes of the Respondents toward Mpox Virus Prevention
Таблица 3. Отношение респондентов к профилактике Mpox
Variables / Вопросы | Frequency (%) / Частота (%) |
Do you believe the Mpox virus can be prevented? Верите ли вы, что вирус Mpox можно предотвратить? | |
Yes / Да No / Нет No response / Нет ответа | 54 (60.0) 24 (26.7) 12 (13.3) |
Which of these preventive measures do you think are effective? Какие из этих превентивных мер вы считаете эффективными? | |
Regular handwashing / Регулярное мытье рук Avoiding contact with an infected person / Избегать контакта с инфицированным человеком Wearing protective devices / Ношение защитных устройств Vaccination / Вакцинация Others / Другое No response / Нет ответа | 16 (17.8) 9 (10.0) 11 (12.2) 27 (30.0) 1 (1.1) 26 (28.9) |
Are you willing to take a vaccine for the Mpox virus? Готовы ли вы сделать прививку от вируса Mpox? | |
Yes / Да No / Нет Not sure / Не уверен No response / Нет ответа | 66 (73.3) 6 (6.7) 6 (6.7) 12 (13.3) |
Do you think healthcare workers in hospitals are adequately trained to manage the Mpox virus? Считаете ли вы, что медицинские работники в больницах достаточно подготовлены к борьбе с вирусом Mpox? | |
Yes / Да No / Нет Not sure No response / Нет ответа | 58 (64.4) 4 (4.4) 13 (14.4) 15 (16.7) |
Concentration of Anti-Mpox Virus IgG Antibody and Seroprevalence by Gender
The seroprevalence of the Mpox virus IgG antibody was 27.4% among females, while it was 9.6% among males. p-value was found to be 0.005, which showed that the Mpox virus is statistically significant among females (Table 4). The concentration of anti-Mpox virus IgG antibody was observed to range from 67.7 pg/mL to 131.4 pg/mL in the blood samples collected from females (Fig. 1), while the concentration of anti-Mpox virus IgG antibody in males ranged from 60.6 pg/mL to 131.8 pg/mL (Fig. 2).
Table 4. Seroprevalence of Mpox virus according to Gender
Таблица 4. Серопревалентность вируса Mpox в зависимости от пола
Variables / Пол | Number examined / Число обследованных | Number of seropositive (%) / Число серопозитивных (%) |
Male / Мужчины | 31 | 3 (9.6) |
Females / Женщины | 62 | 17 (27.4) |
χ2 = 3.854, df = 1, p = 0.050 |
Fig. 1. Concentration of Anti-Mpox Immunoglobulin G Antibody among the females.
Рис. 1. Концентрация антител против Mpox класса IgG среди женщин.
Fig. 2. Concentration of Anti-Mpox Immunoglobulin G Antibody among the males.
Рис. 2. Концентрация антител против Mpox класса IgG среди мужчин.
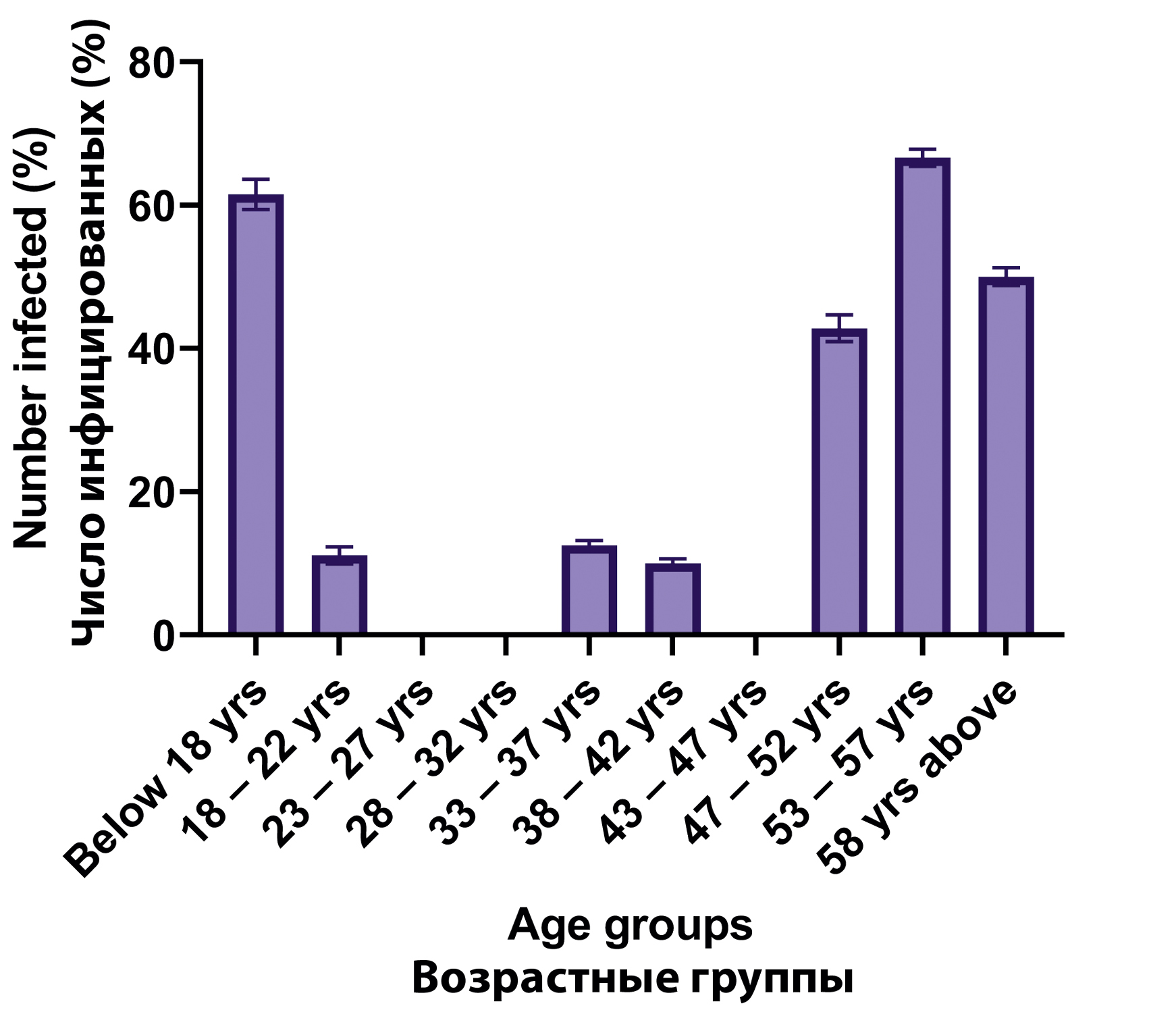
Seroprevalence of Mpox virus by Gender and Age
The seroprevalence of the Mpox virus antibody was higher in the age group ≤ 18 years (61.5%), 53–57 years (66.6%), and ≥ 58 years (50.0%). Moderate prevalence was observed with 43–47 years (42.8%). However, there was no occurrence of Mpox IgG antibody among the 18–27 years and 38–42 years age groups of the respondents. The p-value was found to be 0.000, which showed that anti-Mpox virus IgG antibody occurrence is statistically significant among the children and adults based on the age range (Fig. 3).
Fig. 3. Seroprevalence of Anti-Mpox IgG Antibody according to Age groups.
Рис. 3. Серопревалентность антител класса IgG к Mpox в зависимости от возраста.
Discussion
Mpox is currently not regarded as a public health emergency of international concern; however, it continues to spread in several countries, such as Nigeria. A comprehensive understanding of awareness, knowledge, and control measures for this disease by people is crucial. This study assessed the awareness and seroprevalence of anti-mpox virus IgG antibody among apparently healthy individuals in the community of Ibadan.
This study revealed that the majority of respondents were aware of the Mpox disease, with 61.1% affirming awareness of the disease, which is confirmed in a study by Ogoina et al. [16], who found that 60.5% of participants were aware of Mpox and demonstrated adequate knowledge. However, a notable proportion, 31.1% of the respondents, reported not being aware of the virus in this work. This finding was also corroborated by the report of Olojede et al. [17], where 90.6% were aware of the Mpox, and only 52.2% had good knowledge scores of the disease.
In this study, the respondents frequently indicated that news, family and friends, healthcare workers, and social media were their primary sources of information for awareness; however, broadcasting had a higher percentage among the sources of information. These findings were supported by previous studies conducted by Awoyomi et al. [18], Al-Mustapha et al. [19], and Bakare et al. [20]. In our findings, social media had a second source of information score for the awareness of Mpox disease. Although social media plays a key role in information dissemination, it is attributed to a source of misinformation [21]. This finding was corroborated by the work of Olojede et al. [17], where social media was among the primary sources of information for respondents. Our findings revealed that people are better reached through broadcasting and social media for community intervention during a disease outbreak. Our study also evaluated the knowledge of the participants about the means of transmission of the Mpox virus. Only 48.9% of the respondents understood the methods of transmission of the Mpox virus. Overall, awareness and knowledge of the Mpox disease were generally low, which is similar to the findings of Al-Mustapha et al. [19], who reported low knowledge in a cross-sectional survey on public knowledge of the Mpox in Nigeria.
The attitudinal score of the respondents in this work was observed to be moderate. Our findings showed that 60.0% believed that Mpox could be prevented, and 73.3% expressed willingness to take public vaccination. This report suggests a relatively high vaccine acceptability rate in Nigeria; this report shows little deviation from a similar study conducted in Ghana, where there was 41.7% willingness for public vaccination [22].
In our study, seroprevalence of anti-Mpox virus IgG antibody was observed to be 21.5% among the surveyed population. This seroprevalence is slightly lower compared to the 27.9% seroprevalence reported by Ogoina et al. [16] in a study. However, in another study, Ogoina et al. [23], reported a higher prevalence, where 163 out of 265 cases of anti-Mpox virus antibody were confirmed. Our study showed that the occurrence of anti-Mpox virus IgG antibody can be age dependent, as our study observed higher occurrence of the Mpox among the age groups: ≤ 18 years (61.5%), 53–57 years (66.6%), and ≥ 58 years (50.0%). This finding revealed that the Mpox virus can be common to children and adults, which could be due to the immune status of the age groups. This finding corroborates Mauldin et al. [24], who suggested the Mpox infection was more common among children.
Conclusion
This study revealed a relatively high level of awareness about the Mpox virus among respondents, but there were low knowledge scores about the disease. The discrepancy between awareness and knowledge scores in this study underscores a persistent need for comprehensive public education. The current findings may suggest emerging vulnerability in both pediatric and older adult populations, possibly due to lower immunity, close contact exposure exhibited by these groups, or unvaccinated status following the cessation of routine smallpox vaccination.
Об авторах
John Olusola Olayiwola
Университет Аджайи Кроутер
Автор, ответственный за переписку.
Email: jo.olayiwola@acu.edu.ng
ORCID iD: 0000-0003-2919-0154
канд. биол. наук, старший преподаватель, отделение медицинской микробиологии, кафедра микробиологии и биотехнологии
Нигерия, ОйоAdesuwa Oluwatofunmi Akagbosu
Университет Аджайи Кроутер
Email: Adesuwaakagbosu8@gmail.com
ORCID iD: 0009-0004-0499-6308
бакалавр, лаборант-технолог, отделение медицинской микробиологии, кафедра микробиологии и биотехнологии
Нигерия, ОйоOyindamola John Samson
Университет Аджайи Кроутер
Email: jo.samson@acu.edu.ng
ORCID iD: 0000-0003-0404-7634
магистр, ассистент преподавателя, отделение экологической микробиологии, кафедра микробиологии и биотехнологии
Нигерия, ОйоAdemola Emmanuel Alaba
Университет Аджайи Кроутер
Email: ae.alaba@acu.edu.ng
ORCID iD: 0000-0002-4152-9803
магистр, преподаватель II, отделение медицинской микробиологии, кафедра микробиологии и биотехнологии
Нигерия, ОйоBabalola Sunday Aponjolosun
Университет Аджайи Кроутер
Email: bs.aponjolosun@acu.edu.ng
ORCID iD: 0000-0002-7736-8474
канд. биол. наук, преподаватель II, отделение экологической микробиологии, кафедра микробиологии и биотехнологии
Нигерия, ОйоStephen Ademola Soyemi
Больница университетского колледжа, Ибадан
Email: dcrown1martyr@gmail.com
ORCID iD: 0000-0002-3997-1213
магистр, научный сотрудник I, Диагностический центр PAOOS, кафедра патологии
Нигерия, ИбаданСписок литературы
- Wassenaar T.M., Wanchai V., Ussery D.W. Comparison of Monkeypox virus genomes from the 2017 Nigeria outbreak and the 2022 outbreak. J. Appl. Microbiol. 2022; 133(6): 3690–8. https://doi.org/10.1111/jam.15806
- Harapan H., Ophinni Y., Megawati D., Frediansyah A., Mamada S.S., Salampe M., et al. Monkeypox: a comprehensive review. Viruses. 2022; 14(10): 2155. https://doi.org/10.3390/v14102155
- Mauldin M.R., Andrea M.M., Yoshinori J.N., Anna M., Erin R.W., Whitni D., et al. Exportation of Monkeypox virus from the African continent. J. Infect. Dis. 2022; 225(8): 1367–76. https://doi.org/10.1093/infdis/jiaa559
- Bunge E.M., Bernard H., Liddy C., Florian L., Heinz W., Lorraine R.B., et al. The changing epidemiology of human monkeypox—a potential threat? A systematic review. PLoS Negl. Trop. Dis. 2022; 16(2): e0010141. https://doi.org/10.1371/journal.pntd.0010141
- Nguyen P.Y., Ajisegiri W.S., Costantino V., Chughtai A.A., MacIntyre C.R. Reemergence of human monkeypox and declining population immunity in the context of urbanization, Nigeria, 2017–2020. Emerg. Infect. Dis. 2021; 27(4): 1007–14. https://doi.org/10.3201/eid2704.203569
- Kabuga A.I., El Zowalaty M.E. A review of the monkeypox virus and a recent outbreak of skin rash disease in Nigeria. J. Med. Virol. 2019; 91(4): 533–40. https://doi.org/10.1002/jmv.25348
- Reed K.D., Melski J.W., Graham M.B., Regnery R.L., Sotir M.J., Wegner M.V., et al. The detection of Monkeypox in humans in the Western Hemisphere. N. Engl. J. Med. 2004; 350(4): 342–50. https://doi.org/10.1056/nejmoa032299
- Yinka-Ogunleye A., Aruna O., Dalhat M., Ogoina D., McCollum A., Disu Y., et al. (2019). Outbreak of human Monkeypox in Nigeria in 2017-18: a clinical and epidemiological report. Lancet Infect. Dis. 2019; 19(8): 872–9. https://doi.org/10.1016/s1473-3099(19)30294-4
- Kuebel C., Haskett E. “I’m doing the best I can”: teaching general music in the time of COVID-19. Update Univ. S. C. Dep. Music. 2023; 41(2): 28–37. https://doi.org/10.1177/87551233211067766
- Thornhill J.P., Antinori A., Orkin C.M. Monkeypox virus infection across 16 countries – April-June 2022. Reply. N. Engl. J. Med. 2022; 387(25): e69. https://doi.org/10.1056/nejmc2213969
- WHO. Investigations ongoing into atypical cases of Monkeypox now reported in eight countries in Europe; 2022.
- Ogoina D., Iroezindu M., James H.I., Olumide A.I., Omoleke S., Yinka-Ogunleye A. Monkeypox outbreaks in Nigeria: Epidemiological and clinical features, public health response, and implications for the future. Lancet Infect. Dis. 2022; 22(10): e234–43.
- Bunge E.M., Hoet B., Chen L., Lienert F., Weidenthaler H., Baer L.R. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl. Trop. Dis. 2022; 16(2): e0010141. https://doi.org/10.1371/journal.pntd.0010141
- McQuiston J.H., Braden C.R., Bowen M.D., McCollum A.M., McDonald R., Carnes N., et al. The CDC domestic mpox response – United States, 2022–2023. MMWR Morb. Mortal Wkly Rep. 2023; 72(20): 547–52. https://doi.org/10.15585/mmwr.mm7220a2
- Sharif N., Nazmul S., Khalid J.A., Ibrahim F.H., Fuad M.A., Isabel D., et al. Molecular epidemiology, transmission and clinical features of 2022-mpox outbreak: a systematic review. Health Sci. Rep. 2023; 6(10): e1603. https://doi.org/10.1002/hsr2.1603
- Ogoina D., Inestol O., Adesola Y.O., Chikwe I., Nnaemeka N., Olusola A. Case report: recurrent mpox in a healthcare worker in Nigeria. Am. J. Trop. Med. Hyg. 2023; 109(4): 858–60. https://doi.org/10.4269/ajtmh.23-0232
- Olojede O., Bakare D., Sogbesan A., Salako J., and AA, B. An assessment of awareness, knowledge and perception of monkeypox (mpox) disease among internet users in Nigeria: a cross-sectional survey. Babcock Univ. Med. J. 2024; 7(2): 98–107. https://doi.org/10.38029/babcockuniv.med.j..v7i2.402
- Awoyomi O.J., Njoga E.O., Jaja I.F., Oyeleye F.A., Awoyomi P.O., Ibrahim M.A., et al. Mpox in Nigeria: Perceptions and knowledge of the disease among critical stakeholders-Global public health consequences. PLoS One. 2023; 18(3): e0283571. https://doi.org/10.1371/journal.pone.0283571
- Al-Mustapha A.I., Ogundijo O.A., Sikiru N.A., Kolawole B., Oyewo M., El-Nadi H., et al. A cross-sectional survey of public knowledge of the monkeypox disease in Nigeria. BMC Public Health. 2023; 23(1): 591. https://doi.org/10.1186/s12889-023-15398-0
- Bakare D., Salako J., Sogbesan A., Olojede O.E., Bakare A.A. Assessment of the level of awareness, knowledge, and risk perception of community members about mpox infection in Nigeria. Ann. Ib. Postgrad. Med. 2024; 22(1): 76–87.
- WHO. WHO delivering on its commitment to protect and improve people’s health: stories of healthier populations, access to services and emergency response; 2024.
- Ghazy R.M., Yazbek S., Gebreal A., Hussein M., Addai S.A., Mensah E., Sarfo M., et al. Monkeypox vaccine acceptance among Ghanaians: a call for action. Vaccines (Basel). 2023; 11(2): 240. https://doi.org/10.3390/vaccines11020240
- Ogoina D, Mahmmod M.D., Ballah A.D., Mildred O., Nneka M.C.I., Sebastine O.O., et al. Mpox epidemiology and risk factors, Nigeria, 2022. Emerg. Infect. Dis. 2024; 30(9): 1799–808. https://doi.org/10.3201/eid3009.240135
- Mauldin M.R., McCollum A.M., Nakazawa Y.J., Mandra A., Whitehouse E.R., Davidson W., et al. Exportation of monkeypox virus from the African continent. J. Infect. Dis. 2022; 225(8): 1367–76. https://doi.org/10.1093/infdis/jiaa559
Дополнительные файлы